Chen Khun Lin’, Lyu Tszy Fu
Institute of Oncology and Hospital of Chinese Academy of Medical Sciences
143 patients with greater salivary gland tumors were examined, all of them underwent 3D NLS-graphy, 64 patients underwent non-contrast computed tomography (CT). 78 pleomorphic adenomas were registered in total. In 56 (71.8%) cases, adenomas were located in parotid salivary glands, in 22 (28.2%) cases adenomas were found in submandibular glands. In 46 (82.2%) cases, 3D NLS-graphy presented pleomorphic adenomas of parotid salivary gland as oval or round hyperchromogenic formations with distinct contours and heterogeneous structure. Vascular bed affection was registered in 74 (94.9%) of pleomorphic adenomas cases according to 3D NLS-angiography. Computed tomography presented pleomorphic tumor of parotid salivary glands as high-density single formation (Mavrg = 29,6 ± 4,2 HU) with round shapes, distinct lines and even contours in 44 (93.6%) cases.
3D NLS-graphy demonstrated 100% of sensitivity, 96.3% of specificity and 97.7% of accuracy in detection of pleomorphic adenomas of large salivary glands; CT demonstrated 97.6, 96.4, 97.6% respectively in doing so. 3D NLS-graphy is the main imaging method.
Introduction part
Frequency of large space-occupying lesions of salivary glands in China reaches up to 7% from all diseases of maxillofacilal area. Pleomorphic adenomas are the most common tumors, making from 50% to 65.7% (according to various researches) of all space-occupying lesions of large salivary glands. Diagnostics of such adenomas presents certain difficulties due to uniformity of clinical and instrumental diagnostic signs; as a result, diagnostics error rate varies from 7 to 46%.
The goal of given study is improvement of diagnostics method of large salivary glands pleomorphic adenomas using 3D NLS-graphy and non-contrast computed tomography (CT).
Material and methods
143 patients with tumors of greater salivary glands (age group from 15 to 78 years; mean age = 48.4 ± 2.5 years) were examined to determine the capabilities of given methods. There were 103 women and 40 men patients. All patients underwent 3D NLS-graphy and 64 patients underwent CT of salivary glands procedure.
3D NLS-graphy of salivary glands was carried out according to standard procedures. 3D NLS-graphy was performed using «Metatron»-4025 (IPP, Russia) system with «Golden Dragon» software and the possibility of three-dimensional (3D) visualization of salivary glands.
Intratumoral vascularization was estimated according to 6-point Fleindler’s color scale (from 1 to 6 points) when using 3D NLS-graphy in space-occupying lesions of salivary glands patients. Spectral-entropy analysis was simultaneously performed which allowed estimating the nature of salivary gland neoplasms.
Non-contrast CT of large salivary glands was performed using Ligth Speed (General Electric, USA) and Tomoscan LX (Philips, Germany) scanners in axial projection, scan time 2-5 sec., scanning step – 5 mm., slice thickness – 3 mm. The study was conducted with patients lying on their backs. So-called soft tissue window with the following parameters: window level – from 200 to 300 HU, window width – 50 HU was used as an optimal display and registration mode of tomograms for maximum detailing of salivary glands and surrounding tissues structures.
Results and discussion
We have registered 78 pleomorphic adenomas, which comprised 54.5% of all detected space-occupying lesions of large salivary glands and 63.4% of all benign tumors of large salivary glands. In 56 (71.8%) cases pleomorphic adenomas were located in parotid salivary glands and in submandibular glands in 22 (28.2%) cases.
3D NLS-graphy revealed pleomorphic adenomas of parotid salivary glands in 46 (82.2%) cases as oval or round hyperchromogenic (6 points according to Fleindler’s scale) formations with distinct contours and heterogeneous structure. Surrounding tumor of salivary gland parenchyma was not changed according to its structure and chromogeneity. Pleomorphic adenomas up to 1 cm. in diameter had homogeneous chromogenic structure, adenomas more than 1 cm. had homogeneous isochromogenic structure due to hemorrhage and discharge areas. Pleomorphic adenomas of submandibular glands were characterized by hyperchromogenic foci of various shapes.
3D NLS-angiography revealed vascular bed affections in 74 (94.9%) cases of pleomorphic adenomas. Spectral-entropy analysis was used for differentiation of pleomorphic adenomas from other salivary gland benign tumors (leiomyoma, teratoma, neurinoma).
In 44 (93.6%) cases CT displayed pleomorphic tumor of parotid gland as single high-density formation (Mavrg = 29,6 ± 4,2 HU) of round-shape, with distinct edges and smooth contours. Tumor structure was heterogeneous in 25 (53.2%) and homogeneous in 22 (46.8%) cases. Average tumor size reached 2,9 ± 0,9 cm.; its sizes reached 5.1 cm. if located in deep lobe of gland. The density of unaffected part of parenchyma was 16,4 ± 5,2 HU. In 3 (3.8%) patients, however, tumor had its density equal to surrounding parenchyma, which especially complicated diagnostics of tumors located in the narrow parts of salivary glands (pole).
Unlike parotid glands formations, pleomorphic adenomas of submandibular salivary glands had no clear boundaries separating tumor from gland, tumor density corresponded to parenchyma’s, average tumor size was 3,6 ± 1,3 cm. Thus, significant increase of gland sizes compared to the opposite side and displacement of surrounding soft tissues was registered.
When using NLS-method, most researchers describe pleomorphic adenomas of greater salivary glands as hyperchromogenic (5-6 according to Fleindler’s scale) round-shape formations.
Tumor-surrounding parenchyma of salivary gland was structually and chromogeneically not changed. According to our data, pleomorphic adenomas of submandibular glands (unlike parotid glands tumors), were characterized by isochromogenic foci of various high-chromogeneity forms. Preserved parenchyma was seen at NLS-graphy more clearly compared to CT picture.
In 75% cases of using CT, pleomorphic adenomas had homogeneous pattern; clear, well-determined edges were found in 90% of pleomorphic adenomas, which corresponds to literature data.
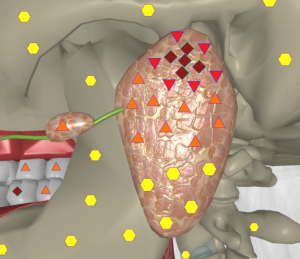
Pic. 1. Computed 3D NLS-graphy of salivary glands.
Pleomorphic adenoma of deep lobe of left parotid salivary gland. A mass of increased homogeneity with distinct contours is spread into an area of pterygomaxillary fossa.
Comparison of CT and NLS-graphy results in diagnostics of salivary glands diseases demonstrated that NLS-graphy with spectral-entropy analysis must be chosen as treatment method in case of tumors because of its high sensitivity, whereas CT must be chosen when dealing with deep-seated tumors for their full three-dimensional detection and determination of facial nerve and tumor ratio, which determines further treatment. We believe that in most cases NLS-graphy is sufficient for preliminary neoplasms diagnosing, CT is used in case of deep lobe affection or suspected malignant process. Intravenous enhancement during CT is useful in non-glandular formations (especially those located in peripharyngeal space) for detection and localization of masses in relation to carotid artery or jugular vein.
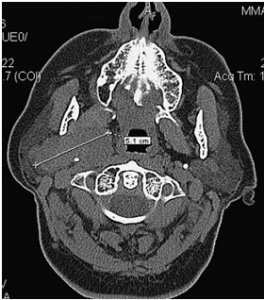
Pic. 2. Computed tomogram of salivary glands.
Pleomorphic adenoma of deep lobe of right parotid salivary gland: a mass of increased density with strict contours, sized 5.1 x 2.6 cm, spreads into a pterygomaxillary fossa area.
In case of formation more than 3 cm in diameter (regardless of its nature and localization) it is always necessary to use computer tomography to obtain accurate data on tumor spread into the surrounding tissues. 3D NLS-graphy demonstrated 100% sensitivity, 96.3% specificity, 97.7% accuracy, CT showed 97.6, 96.4 and 97.6%, respectively in detection of pleomorphic adenomas of large salivary glands.
Conclusion
Thus, examination analysis of complex patients with space-occupying lesions of salivary glands had shown that 3D NLS-graphy is leading visualization method.
It allows clarifying size, structure, shape and tumor type using spectral-entropy analysis. Computer tomography is used in evaluation of tumors more than 3 cm. in diameter; it provides accurate estimation of volume, structure of tumor and condition of adjacent anatomical structures.
References
1. Bialek E.J., Jakubowski W., Karpinska G. Role of 3D NLS-graphy in Diagnosis and Differentiation of Pleomorphic Adenomas. Arch. Otolaryngol. Head Neck Surg. 2013; 123: 829–833.
2. Yousem D.M., Kraut M.A., Chalian A.A. Major salivary gland imaging. Radiology 2000; 216: 19–29.
3. Cheng H.L., Djong S.L, et al. Neither MRI, CT nor US superior to diagnose tumors in the salivary glands – an extended case study. Head & Face Medicine 2011; 4: 19.
4. Alyas F., Lewis K., Williams M. et al. Diseases of the submandibular gland as demonstrated using High Resolution Ultrasound. Br. J. Radiol. 2005; 78: 362–369.
5. Lee H.C. Imaging of salivary gland tumours. Cancer Imaging 2009; 7: 62–68.
6. Mendenhall W.M., Mendenhall C.M., Werning J.W. et al. Salivary Gland Pleomorphic Adenoma. Am. J. Clin. Oncol. 2008; 31: 95–99.
7. Jang M., Park D., Lee S.R. et al. Basal Cell Adenoma in the Parotid Gland: CT and MR Findings. Am. J. Neuroradiol. 2004; 25: 631–635.
8.Yasumoto M., Shibuya H., Suzuki S. et al. Computed tomography and ultrasonography in submandibular tumours. Clin.Radiol. 1992; 46: 114–120.
9. Nesterov V.I. «Computer non-linear diagnostics»//Collection of scientific works of Institute of Practical Psychophysics «Topical issues of NLS-diagnostics». Volume I. M.: Book, 2006, p. 5-6
10. Nesterov V.I. «3D NLS diagnostics. Prospects for development»// Collection of scientific works of Institute of Practical Psychophysics «NLS-technologies in medicine – development prospects». Volume III. M.: Book, 2010, p. 5-8
