Pak Yun Tek, Kim Gi Song
Medical center ASAN
Structural-degenerative, age-related changes are usually considered as irreversible in case of osteoarthrosis in later stages. Identification and evaluation of NLS-manifestation signs of osteoarthritis provide understanding of its causes and features of its further progression. Determination of interrelations of structural changes in joint at different disease stages (early stages especially) assists in effective treatment policy planning. Given article presents study of clinical significance and diagnostic efficiency of early NLS-manifestations of knee osteoarthritis that took place in the Republic of Korea.
Introduction part
NLS of knee joints may establish itself as a leader in modern diagnostics of articular pathology. Possibilities of modern rheumatology and orthopedics (that possess variety of therapy methods and means) require accurate and timely diagnostics of pathological process origins, especially in early stages of disease. In the first place, it concerns such pluricausal diseases like osteoarthritis; one of its most common forms is knee-joint osteoarthritis. Abundance of risk factors (including genetic ones) does not always allow timely identification of osteoarthritis development and its early manifestations signs, especially in case of obliterated symptoms. Application of large amount of modern therapeutic agents in early stages provides both ceasing of disease progression and reversal of degenerative changes development (hyaline cartilage particularly).
In this regard, early diagnostics of initial osteoarthritis manifestations becomes especially urgent. Radiography of joints remains the most spread method of osteoarthritis diagnostics, however initial osteoarthritis manifestations cannot be revealed by given method. Perfection of technology and accumulated experience demonstrates the advantage of NLS of joints compared to other ray-methods. In addition to its high information value, NLS is affordable, mobile and safe diagnostics method that provides easy and dynamic observation; but literature data analysis shows that method’s potential in detection of early pre-radiological knee-joint osteoarthritis is discovered not completely.
Research objective: detection of NLS-manifestations of nontraumatic knee-joint osteoarthritis in pre-radiological and I-II radiological (Rg) stages and evaluation of their sensitivity, specificity and clinical significance.
Patients data with various Rg-stages of knee-joint osteoarthritis
|
Characteristics |
Control group |
General group |
||
|
0 Rg |
I Rg |
II Rg |
||
|
N of patients Men Women Diagnostic-treatment artroscopy
KOOS Age, years Cartilage degenerative thinning index Osteophytosis, mm. Exudate, mm. |
40 24 16 0
0 41 ± 4.7 0.79 ± 0.03 0 2.2 ± 0.03 |
85 48 37 39
29 ± 5.3 46.3 ± 3.5 0.76 ± 0.03 0.72 ± 0.08 3.4 ± 0.02 |
20 12 8 13
46 ± 12.3 47.1 ± 7.4 0.64 ± 0.07 1.44 ± 0.22 3.9 ± 0.1 |
20 9 11 12
61.5 ± 17.4 51.2 ± 11.3 0.53 ± 0.07 2.16 ± 0.26 4.4 ± 0.7 |
|
Cartilage degradation maximum degree, % from group |
||||
|
0 I II III IV |
100 0 0 0 0 |
14 79 7 0 0 |
0 60 25 15 0 |
0 30 50 20 0 |
|
Cartilage degradation dominant degree, % from group |
||||
|
0 I II III IV |
100 0 0 0 0 |
88 12 0 0 0 |
75 25 0 0 0 |
50 35 15 0 0 |
|
Chondromalacia of kneecap medial fasing, % from visualization group (0 Rg-stage – 66 out of 79 patients, I Rg-stage – 16 out of 19 patients, II Rg-stage – 12 out of 12 patients) |
||||
|
0 1 type 2 type 3 type |
100 0 0 0 |
16 61 23 0 |
16 47 26 11 |
0 42 42 16 |
|
Degenerative changes manifestation rate of medial meniscus, % from group |
||||
|
0 I II |
0 0 0 |
87 13 0 |
85 10 5 |
45 35 20 |
|
% from group |
||||
|
Kneecap lateroposition Enthesopathies Hoffa’s body hypertrophy Mediopatellar fold V-shaped patellar (knee) plateau |
7.5 0 0 0 0 |
33 8 11 12 3.5 |
30 20 10 5 0 |
20 30 15 10 5 |
Material and methods
«Metatron»-4025 (Institute of Practical Psychophysics, Russia) system was used in our research. «Red Dragon» professional software with possibility of 3D-visualization of images and microscans examination potential was used together with «Metatron» system.
The research was performed in 125 patients, age group from 40 to 65 years, suffering from knee joint pains during 1 to 5 years (general group) at relative clinical remission stage, without injuries and knee joint operative treatment in their medical history. Control group consisted of 40 men and women from 25 to 35 years without clinical (0 points according to KOOS scale) and instrumental signs of knee-joint osteoarthritis.
All patients underwent clinical examination with semiotics summation according to KOOS scale, Rg examination and NLS-examination of the knee within research procedure. 64 patients underwent medical-diagnostic arthroscopy (its entrance showed no significant injuries of infra-articular structures) due to persistent pain symptoms.
General group was divided into subgroups according to Rg-osteoarthritis stages. Patients of III and IV Rg-osteoarthritis stages were not included into research (see. Table).
The following factors were examined during NLS-research: structure and thickness of hyaline cartilage of femoral condyles, degenerative changes in menisci, medial facet of kneecap, kneecap condition, fat body and alar folds structures, mediopatellar folds condition, presence and localization of osteophytes and structure of tendon-ligamentous apparatus.
Results and discussion
In accordance with Rg-picture, 85 patients had no osseous changes; 20 patients had I stage knee-joint osteoarthritis and 20 patients had II stage knee-joint osteoarthritis. Total score according to KOOS scale in patients with 0 Rg knee-joint osteoarthritis stage was significantly higher than in control group, and significantly lower than in patients with II Rg knee-joint osteoarthritis stage.
Hyaline cartilage of femoral condyles
Status and structure of cartilage on condyles anterior surface, on load-bearing face of condyles when flexing knee at 70-90° angle and also cartilage thickness of condyles rear surface was estimated.
We evaluated cartilage condition in anterior and load-bearing faces against maximum thickness of cartilage rear surface of corresponding condyles (cartilage degenerative thinning index) considering prevalence of degenerative cartilage thinning of anterior and load-bearing condyles faces relative to posterior ones where hyaline cartilage remains relative secure for prolonged periods. Statistical analysis considered the minimum index value out of 4 values (the one received from joint cartilage degenerative thinning index).
Structural changes of hyaline cartilage were evaluated according to the classification close to ICRS (International Cartilage Repair Society) classification. But this classification was supplemented and modified by us for NLS-diagnostics:
0 – normal cartilage;
I degree – chromogeneity increase (3-4 points according to Fleindler’s scale), homogeneous structure, clear moderately irregular contour;
II degree – chromogeneity increase (4-5 points according to Fleindler’s scale), heterogeneous structure, indistinct irregular contour, cartilage degenerative thinning index > 0.5;
III degree –chromogeneity increase (5-6 points according to Fleindler’s scale), expressed heterogeneous structure, indistinct irregularly-marked eroded contour, cartilage degenerative thinning index < 0.5, deformation of subcartilaginous growths, calcification areas;
Maximum and prevailing degrees of structural changes were estimated.
Minimal cartilage degenerative thinning index in control group was significantly different from the one in general group: 0.79 ± 0.03 against 0.64 ± 0.04 (p <0.05), including I and II Rg-stage subgroups of knee-joint osteoarthritis, but it did not differ from patients with pre-radiological stage of knee-joint osteoarthritis.
Qualitative structural changes of hyaline cartilage registered in majority of general group patients including pre-radiological stage; maximum degenerative changes reached II manifestation rate in 7% of patients. No structural changes of hyaline cartilage condyles found in 12 general group patients.
In accordance with data obtained, manifestation rate of NLS-picture degenerative changes, both maximum and predominant, was significantly higher in general group compared to control group, including 0 Rg-stage knee-joint osteoarthritis subgroup. Accurate positive correlative relation between manifestation rate of degenerative changes and Rg-stage of knee-joint osteoarthritis (maximum and prevailing respectively – 0,58 and 0,75, p <0,05) was registered.
Comparison of NLS-picture with data of diagnostic-treatment artroscopy had revealed the following: sensitivity of NLS in cartilage changes diagnostics in detection-available parts consisted 87.7%, specificity – 82.35%, prognostic positive result – 95%, prognostic negative result – 63.64%.
Chondromalacia of kneecap medial facet
Manifestation degree of kneecap medial facet chondromalacia (in addition to the abovementioned criteria typical for degenerative changes in cartilage as a whole) was estimated according to the area of often-revealed hyperchromogenic spot in the facet’s center. Given phenomenon reflects chondromalacia of cartilage basal layers typical for thick hyaline cartilage of kneecap.
We received NLS-images spot at 3D-visualization of microscans with passing of scanning image plane deep into patellofemoral joint, parallel to anterior surface of medial femoral condyle.
Such degeneration type of certain intensity degree was found in 94 general group patients; 15 patients had no changes.
Several types of NLS- degeneration manifestations were found:
1st type – diffuse increase of basal layer chromogeneity with no distinct edges;
2nd type – homogeneous hyperchromogenic area with clear smooth contours – centrally or eccentrically located, accompanied in some cases by common chromogeneity moderate increase;
3rd type – central spot heterogeneity with calcification elements and hypochromogenic inclusions; in some cases small linear hyperchromogenic inclusions of microcracks.
Registration of such changes in the majority of patients with 0 Rg-stage of knee-joint osteoarthritis draws an attention. Structural changes of hyaline cartilage of kneecap medial facet are distinctly detected more often and more apparent as disease progresses in the form of radiographic picture change.
NLS sensitivity in chondromalacia diagnostics was 88.29%, specificity – 98.55%, positive predictive result – 98.99%, negative predictive result – 83.95% when comparing NLS-picture with diagnostic-treatment artroscopy data.
Osteophytosis
Acentric osteophytosis is a typical Rg-osteophytosis manifestation; it is detected by NLS at its earliest manifestations when osteophytes height reaches 0.5 mm. Osteophytes are as well as available for detection during NLS in spots requiring the use of special additional Rg-planes (patellofemoral joint in particular). Acentric osteophytosis was registered in all general group patients, including Rg-0 stage patients and in this case it served as general diagnosis criterion.
Increase of osteophytes intensity during NLS was confirmed by significant indices differences among all subgroups with 0, I and II Rg-stages (p <0,05) was registered as Rg-picture progressed. Location of osteophytosis of maximum intensity was registered in patellofemoral joint compared to tibiofemoral joint in patients with 0 and I osteoarthrosis Rg-stages (in majority of cases: 80 and 85% respectively).
Degenerative changes of menisci
Medial meniscus degeneration occurred in 13% of general group patients during our research. No degenerative changes of lateral meniscus were found (except for 2 cases of discoid meniscus).
We have developed the following working classification due to practical needs of severity determination of meniscus degeneration and lack of standard classification:
0 – no visible changes;
I stage – uneven chromogeneity increase, irregular indistinct contour;
II stage – + contour bulging outside the articular surface, hyperchromogenic layers;
III stage – + visible zone defects, perimeniscal edema, vascular bed affection revealed by NLS-angiography;
Degenerative changes (up to III intensity degree inclusively) were revealed during our research. Prevalence of meniscus degenerative changes in III Rg-stage of knee-joint osteoarthritis patients was significantly higher than in 0 and II Rg-stage of knee-joint osteoarthritis patients, p <0,05. Degenerative thinning of hyaline cartilage of load-bearing surface of medial femoral condyle (cartilage degenerative thinning index 0,38 ± 0,11 against 0,62 ± 0,06, p <0.05) was revealed in II Rg-stage patients subgroup and degenerative changes of medial meniscus compared to patients with no such changes.
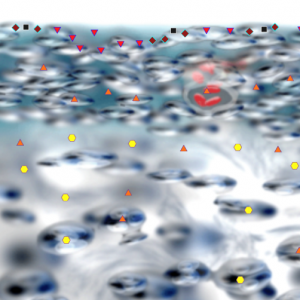
Pic. 1. 3D-ultramicroscanning of a hyaline cartilage.
I degree of intercondylic hyaline cartilage degenerative changes,
Areas of local chromogeneity increasing.
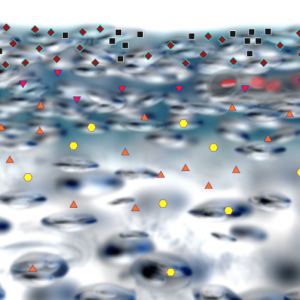
Pic. 2. 3D-ultramicroscanning of a hyaline cartilage.
II degree of intercondylic hyaline cartilage degenerative changes,
extensive superficial damage of a cartilage.
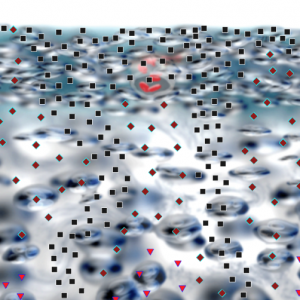
Pic. 3. 3D-ultramicroscanning of a hyaline cartilage.
III degree of intercondylic hyaline cartilage degenerative changes, severe diffuse damage of a cartilage to its depths, with areas of destruction.
Discoid lateral meniscus
During our study given disorder was found in 2 patients with II and III Rg-stages of knee-joint osteoarthritis; these patients also had evident degenerative changes of hyaline cartilage of load-carrying surface of lateral femoral condyle. Both cases confirmed by diagnostic-treatment artroscopy.
Relatively high NLS diagnostic significance in diagnostics of knee-joint osteoarthritis having both high sensitivity/specificity of method and wide range of registered pathological changes was revealed in the course of study. Manifestations of osteoarthrosis vary and in most cases they start developing not with bone changes detected by radiography. Changes of hyaline cartilage, small osteophytes are detected during NLS and at pre-radiological stage of knee-joint osteoarthritis, simultaneously with clinical semiotics manifestation. Many manifestations, if not reversible, but quite effectively stabilized by modern therapeutic agents at this stage of disease. This approach greatly improves the clinical significance of nonlinear diagnostics in early detection of described signs of intra-articular degeneration. When using NLS, structural changes of hyaline cartilage are detailed visible and determination of localization of its most evident structural changes becomes possible, which often shows primary cause of knee-joint osteoarthritis development, especially in case of apparent asymmetric affection of lateral and medial parts. Certain structural changes often occur in combination that promotes some characteristic symptom groups such as: combination of kneecap lateroposition, degenerative thinning of anterior surface of lateral femoral condyle, enthesopathy and calcification of the lateral parts of quadriceps tendon. Detection and presentation of acentric osteophytosis is both important at pre-radiological stage of knee-joint osteoarthritis and at later stages, because (as our research had shown) patellofemoral arthrosis becomes predominant in early stages; standard radiographic views show such arthrosis not sufficiently clear. Minor structure anomalies of knee joint, such as kneecap lateroposition, hypertrophy of fat body and alar folds, mediopatellar fold and etc., have important practical importance since they may contribute to osteoarthritis development (especially patellofemoral one) while menisci anomalies, discoid meniscus in particular, and also their degenerative changes cause predominance of dissymmetric tibiofemoral arthrosis.
Conclusions
1. Nonlinear diagnosis is an important instrumental diagnostic method of knee-joint osteoarthritis, especially in its early stages, when there is no radiological semiotics.
2. NLS-criteria of hyaline cartilage affection provides sufficient sensitivity and specificity in comparison with diagnostic-treatment artroscopy data.
3. Determination of typical NLS-symptom groups including topical localization of hyaline cartilage structural changes and corresponding affections of associated articular structures provides establishing of osteoarthritis development causes and adequate choice of treatment.
4. NLS provides revealing of structural abnormalities of formation and development of knee-joint that promote osteoarthritis development. This factor determines their presence evaluation necessity and manifestation degree within standard research.
5. We have developed working classifications of NLS picture of degenerative changes of hyaline cartilage, menisci, and degenerative thinning of cartilage index. These classifications assist in overall intensity assessment of knee-joint osteoarthritis and planning of treatment policy features.
References
1. Hiroshi Kuroki, Yasuaki Nakagawa, Koji Mori et al. NLS properties of articular cartilage in the tibio-femoral joint in knee osteoarthritis relation to clinical assessment (International Cartilage Repair Society grade). Arthr. Res. Ther. 2013; 10 (4): 65.
2. Brittberg M., Peterson L. Introduction to an articular cartilage classification. ICRS Newslett. 1998; 1: 8.
3. Schmidt W.A., Schmidt H., Schicke B. et al. Standard reference values for musculoskeletal NLS-graphy. Ann. Rheum. Dis. 2013; 65: 988–994.
4. Petrov M.S., Voroshilova L.A., Kartuzov V.M., Vesnin A.Ya., Derevyanko G.V., Guglya A.P. «NLS-research in assessment of knee-joint condition in case of deforming osteoarthrosis»// Collection of scientific works of Institute of Practical Psychophysics «Topical issues in NLS-diagnostics». Volume I. M.: Book, 2006, p. 47-50.
5. Nesterov V.I. «3D NLS diagnostics. Prospects for development»// Collection of scientific works of Institute of Practical Psychophysics «NLS-technologies in medicine – development prospects». Volume III. M.: Book, 2010, p. 5-8
