T.Clark, A.Perry, S.Collins
St.Paul University Hospital of Dallas
Introduction
At the present moment liver transplantation is the only radical method of treatment at terminal stages of chronic diffuse diseases of liver. One of the most promising options of liver transplantation in case of deficiency of cadaveric “imported” organs is a transplantation of liver right love acquired from alive relative donor. The advantages of right lobe of liver using as a transplant are: constant anatomic structure of arterial and portal blood supply of a right lobe; greater diameter of right branch of hepatic artery and so it is more convenient for anastomosing; configuration of a right lobe is more convenient for placing in a recipient’s organism and it excludes a possibility of transplant moving in abdomen during post-operative period; resection of donor’s liver limited by hernihepatectomy volume, at the same time medial vein remains as a part of donor’s liver. So this intervention is more attenuated anatomically, than using of a left lobe.
In medical practice comprehensive NLS-study is regarded as one of the most promising methods of hardware diagnostics and monitoring. At the present moment the experience of liver transplantation from alive relative donors is not sufficient, and available references are based on practice on rare transplantation centers where this method is applied. Works on possibilities of integrated NLS-study in evaluation of liver transplant condition and dynamic monitoring of patients during posttransplant period are missing in modern literature. All this has become a reason for carrying out of the present study.
The objective of this work is identifying of NLS criteria for evaluation liver right lobe transplant condition at various periods after transplantation.
Material and methods
Materials for this work are the results of comprehensive NLS-study of 70 patients are relative transplantation of liver right lobe. Follow-up period was from 1 month to 6.5 years (23.5±20.7 months on average). Average age of recipients was 20±13 years (7-61 years old patients). Among them there were 39 children (22 boys and 17 girls) aged 7-16 (12.4±3 on average) and 31 adult (13 men and 18 women) aged 17-61 (30.6±14.3 on average). Distribution of patients in accordance to nosological forms was the following:
|
Nosological forms of liver affection |
Number of cases (%) |
|
Liver cirrhosis as a result of Wilson’s disease |
30 (42,9) |
|
Liver cirrhosis as a result of primary sclerosing cholangitis |
10 (14,3) |
|
Liver cirrhosis of viral etiology |
6 (8,6) |
|
Primary biliary cirrhosis |
6 (8,6) |
|
Liver cirrhosis as a result of Byler disease |
3 (4,3) |
|
Liver cirrhosis as a result of Caroli disease |
3 (4,3) |
|
Liver cirrhosis as a result of biliary hypogenesis |
3 (4,3) |
|
Liver cirrhosis as a result of autoimmune hepatitis |
2 (2,9) |
|
Secondary biliary cirrhosis |
2 (2,9) |
|
Liver cirrhosis as a result of Chiari disease |
2 (2,9) |
|
Liver cirrhosis as a result of AIAT deficiency |
1 (1,4) |
|
Liver congenital abnormality with development of liver cirrhosis |
1 (1,4) |
|
Hepatocellular carcinoma |
1 (1,4) |
|
Total: |
70 (100) |
Comprehensive NLS was carried out with Metatron-4027 device (ClinicTech Inc., USA; IPP, Russia) with high-frequency generator of 9.6 GHz, unit of continuous spiral scanning and professional software Metapathia GR Hospital allowing to carry out three-dimensional visualization of liver.
During examination we used NLS-ultramicroangioscanning mode and spectral-entropic analysis (SEA), allowing to detect spectral similarity of morphological structures of hepatic parenchyma and vessels with digital models of etalon processes of healthy and pathologically changed tissues.
The first NLS was carried out after completing of surgery in intensive care unit. Within the first week after surgery NLS was carried out every day. At positive course of posttransplant period, during the second week NLS was carried out every second day, and then once in a week until discharge from a hospital. If necessary, minimally invasive manipulations were carried out with NLS monitoring. After discharge from a hospital NLS-monitoring was carried out once in 3-4 months, in case of indications – more frequently.
Integrated NLS of liver right lobe transplant was carried out in accordance with created by ourselves protocol and in included evaluation of transplant’s parenchyma, vessels and intrahepatic bile ducts condition. During monitoring period all recipients were subjected to NLS-ultramicroscannng with SEA of hepatic parenchyma. Results of integrated NLS were supplemented with data of morphological, endoscopic and x-ray researches.
Results
On the basis of data acquired during this study we have developed criteria for liver right lobe transplant condition evaluation, reflecting positive course of posttransplant period. At that we evaluated condition of transplant parenchyma, vessels and intrahepatic bile ducts. Intensity of liver right lobe transplant parenchyma chromogeneity at non-complicated course of post-transplant period was equal or slightly higher than chromogeneity of left lobe and was less than 3-4 points at Fleindler’s scale.
After evaluation of liver right lobe transplant parenchyma condition, we divided detected changes of chromogeneity into diffuse and local. In its turn local changes were divided into regional and focal. Diffuse changes of liver right lobe transplant parenchyma included equal increasing of chromogeneity detected in all areas. Regional changes included increasing of liver right lobe transplant parenchyma’s chromogeneity, detected in one or several segments, without changing of liver tissue’s morphological structure.
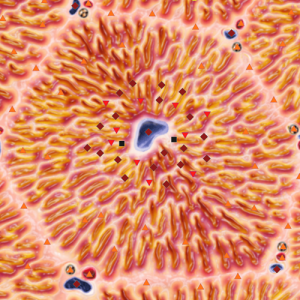
Pic. 1. NLS-ultramicroscanning of liver tissue. Regional increasing of chromogeneity of liver right lobe transplant parenchyma in early post-transplant period in an area of VI segment.
Diffuse increasing of liver right lobe transplant parenchyma chromogeneity was detected only in late post-transplant period in 5 (7.1%) patients and was conditioned by development of transplant’s dysfunction.
Regional changes of liver right lobe transplant parenchyma chromogeneity in early post-transplant period (30 days) were registered in 3 (3.4%) recipients and were represented by increasing of chromogeneity in an area of VI and VII segments of liver. During late post-transplant period regional changes of liver right lobe transplant parenchyma chromogeneity were detected in another 3 (3.4%) recipients, however in this case we saw increasing of chromogeneity in an area of VI and VII segments of a transplant.
Focal changes of liver right lobe transplant parenchyma were detected in late post-transplant period in 3 (3.4%) patients. In all cases it was acute abscesses, accompanied by intensive increasing of chromogeneity (6 points at Fleindler’s scale) in a nidus.
NLS-signs of hepatic artery thrombosis were detected by NLS-ultramicroangiography in 1 (1.4%) patient during early post-operative period.
Hepatic artery stenosis in early post-operative period was diagnosed in 1 (1.4%) patient, and in another patient in late post-operative period. In both cases NLS data were confirmed by SEA results.
Non-occlusive thrombosis of portal vein in early post-operative period was diagnosed in 1 (1.4%) patient on the basis of SEA of morphological structure of thrombus in an opening of posterior branch of right portal vein, which did not close opening of this vessel completely.
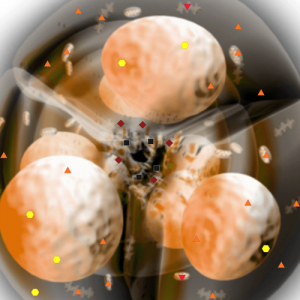
Pic. 2. Portal vein obturating thrombosis in late post-operative period.
Portal vein stenosis is in an area of portal anastomosis formation according to a data of NLS-ultramicroangiography with SEA.
Inferior vena cava stenosis was diagnosed by NLS with SEA in early post-operative period in 1 (1.4%) recepient, subjected to surgery because of liver cirrhosis developed due to Chiari disease.
Signs of biliary hypertension in a form of intrahepatic bile ducts affection, accompanied by increasing of chromogeneity, were detected in 23 (32.9%) patients in early post-operative period. Among them moderate changes of intrahepatic bile ducts (4-5 points) were diagnosed in 21 patient, when significant changes of intrahepatic bile ducts (6 points) – in 2.
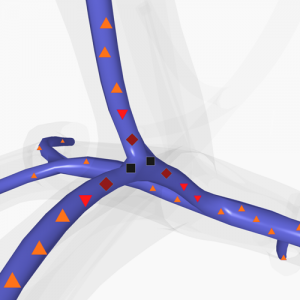
Pic. 3. NLS-ultramicroscanning of interlobular bile duct.
Biliary sludge in an opening of destructively changed interlobular bile duct.
According to NLS data, in late post-operative period affection of intrahepatic bile ducts was revealed in 46 (65.7%) of recipients. Moderate changes of intrahepatic bile ducts (4-5 points) were diagnosed in 27 patient, significant changes (6 points) – in 19 recipients.
Discussion
At the present moment in references there is no such concept as regional changes of transplant parenchyma chromogeneity at NLS-studies. Parenchymatous complications are divided into focal and diffuse, but we believe that introduction of concept of regional changes of parenchyma chromogeneity allows to characterize changes detected by NLS more accurately. Also there is no data regarding frequency of parenchymatous complications development.
In our monitoring diffuse increasing of liver right lobe transplant chromogeneity was registered in 5 (7.1%) patients in late post-operative period. Revealed changes were accompanied by increasing of transaminase, cholestasia enzyme and bilirubin levels and were conditioned by development of transplant dysfunction. We believe that NLS with SEA allows to identify a reason of transplant parenchyma diffuse changes development in majority of cases. NLS with SEA data is confirmed by results of clinical and laboratory studies and materials of morphological research of liver biopsy material in 98.6% of cases.
Regional changes of liver right lobe transplant parenchyma chromogeneity detected in 3 (4.3%) recipients in early post-transplant period and in 3 (4.3%) recipients in late post-transplant period were not accompanied by transplant dysfunction development and retrospectively were regarded as a consequence of regional disorders of blood circulation in mentioned segments. There are no references about this issue, so our assumptions require further study.
Revealing of liver right lobe transplant parenchyma chromogeneity focal changes (4.3%), in our research it were acute abscesses, promoted identification of reasons of pyretic fever, increasing of cytolysis and cholestasis enzymes and helped to define tactics of further treatment.
Detected NLS-signs of hepatic artery thrombosis confirmed during relaparotomy applied in order to reconstruct arterial anastomosis. According to our data percentage of this serious complication is lower than in studies of our colleagues, who report about higher frequency of hepatic artery thrombosis development, equal to 1.7% – 26%. It can be explained by improving of surgical technique of arterial anastomosis application.
Detection of hepatic artery stenosis in early post-transplant period promoted choosing of further treatment tactics (prescription of heparin to prevent hepatic artery thrombosis development).
Revealing of various forms of portal anastomosis (thrombosis of portal vein anterior branch – 1.4%, portal vein stenosis in area of anastomosis application – 2.9%) and inferior vena cava (inferior vena cava stenosis – 1.4%) did not require using of specifying methods of investigation.
In our studies biliary complications of relative transplantation had leading position among others, which corresponds to opinions of foreign scientists.
The main problem of late post-transplant period is affection of intrahepatic bile ducts, caused by formation of biliary anastomosis strictures. According to NLS data, 11 biliary reconstructions were carried out in 8 (11.4%) patients because of biliary anastomosis strictures.
Conclusion
Integrated NLS study, including three-dimensional scanning, NLS- ultramicroscanning with SEA and NLS-ultramicroangiography, is a prospective hardware method allowing ot evaluate condition of liver transplant during various stages of post-transplant period accurately and in proper time.
NLS of liver transplant may become the main method bile ducts condition monitoring, allowing to diagnose biliary complications accurately, and to evaluate possibilities of treatment-diagnostics minimally invasive manipulations and dynamically monitor efficiency of applied treatment.
References
1. Carithers R.L.J. Liver transplantation // Liver transplantation. – 2000. – Vol. 6, N1. – P. 122-135.
2. Gautier S., Tsiroulnicova O., Filin A. et al. Right hepatic lobe for living related grafting // Hepato-Gastroenterology. – 1998. – Vol. 45. – Suppl.II. – P.CCCLXXX.
3. Marcos A., Fisher R.A., Ham J.R. et al. Right lobe living donor liver transplantation. // Transplantation. – 1999. – Vol. 68(6). – P. 798-803.
4. Hussain H.K., Nghiem V.H. Imaging of hepatic transplantation // Clinics in liver disease. – 2002. – Vol. 6 (1).
5. Miller C.M., Gongolesi G.E., Florman S. et al. One hundred nine living donor liver transplants in adults and children: a single.center experiance // Annuls of Surgery. – 2001. – Vol. 234. – N 3.
6. Dalgic A., Dalgic B., Demirogullari B. et al. Clinical approach to graft hepatic thrombosis following living related liver transplantation // Pediatr.Transplant. – 2003. – Vol. 7(2). – 149-52.
7. Ishiko T., Egawa H., Kasahara M. et al. Duct-to-duct biliary reconstraction in living donor liver transplantation // Ann Surg. – 2002. – Vol. 236(2). – P. 235-40.
8. Tokar S.P., Davydova А.S., Guseva Т.L., Gusarov V.I., Khabibullina Z.F., Pugacheva L.S. Non-linear computed diagnostics and question of hepatopancreoduodenal area pathology // Collection of scientific works of the Institute of Practical Psychophysics “Actual aspects of NLS-diagnostics”. Volume I. М.: Katalog, 2006, p. 77-88.
9. Shvack А.Y., Nesterov V.I., Ogluzdina N.L. Certain aspects of NLS-diagnostics of focal pathologies of liver // Collection of scientific works of the Institute of Practical Psychophysics “NLS-technologies in medicine – prospects of development. Volume III. М.: Katalog, 2010, p. 13-19.
