S.P.Mironov, S.V.Komarovsky, V.P.Kurepin
Central scientific research institute of traumatology and orthopedy named after N.N.Priorov, Moscow
The article presents a detailed description of clinical and NLS-pictures of the peripheral neurofibromatosis of the 2nd type. In 60.0% of cases neurofibromas have been manifested by single neoplasms which were located hypodermically and intramuscularly, mainly on extensor surfaces of a body and extremities, and have not been connected with the main nervous trunks. In 40.0% of cases it was located along the main nervous trunks and plexuses. Neurofibromatous nods looked like hyperchromogenic neoplasms of oval or roundish shape, homogeneous structure, with even contour. NLS-angiography registered misperfusion in 66.7% of cases. Results of NLS-ultramicroscanning with SEA have been verified by morphological research of removed tumors.
INTRODUCTION
Neurofibroma (fibroneuroma) is a benign tumor of a peripheral nerve developing from Schwann cells and fibroblasts, more often located on a surface, in depth or under a layer of hypoderm. Single neurofibromas are extremely rare as independent nosological unit. More frequently presence of neurofibromas is a sign of a hereditary disease – neurofibromatous.
In 1822 Scottish surgeon Wishart J.H. for the first time has described neurofibromatous of 2nd type (NF2). In 1882 von Recklinghausen F.D. has studied and described neurofibromatous of 1st type (NF1). Despite distinctions in the description of diseases, Cushing H.W. in 1916 in the scientific work has united them under a single name “Recklinghausen disease”. Only after many years, after molecular genetic testing, results of which have been published in 1985 and 1987, basic differences in pathogenesis of NF1 and NF2 have been revealed. It has been proved that these are absolutely different diseases demanding different diagnostic and medical tactics.
Scientific references have descriptions of 8 types of NF, however majority of them, except NF2, are considered to be an abortive form of NF1 and are not considered as independent nosological forms. Exceptions are segmentary NF (NF of 5th type) (NF5) at which typical displays of NF1 are located in one or several neighboring dermatomes (registered extremely seldom, usually it is not inherited), and not included into number 8 spinal NF at which all spinal roots are affected symmetrically (several observations are described).
NF2, as well as NF1, is an autosomal dominant disease. In patients NF2 is registered less often, than NF1, in 1 of 50000 newborns. Gene NF2 is located in 22th chromosome (22q12) and codes synthesis of tumoral growth suppressor – merlin protein, or schwannomin which functions as membranous organizer and provides, first of all, construction and functioning of a cellular skeleton. This protein has the greatest importance for proliferation regulation of cells with neuroectodermal origins. If NF2 allelic gene is damaged due to symmetric mutation or loss of heterozygosity in 22nd chromosome, synthesis of normal merlin in a cell stops, dynamic balance of growth regulation is shifted to proliferation, and therefore benign tumoral growth appears. NF2 gene has high penetrance. Practically in all of its carriers the disease develops by 60 years. Developing at NF2 tumors are benign, but more biologically aggressive, than at NF1.
Neurosurgeons and traumatologists-orthopedists at diagnosing base mainly on clinical manifestations of a pathology, anamnestic data and results of patient check-up, however it is not enough for revealing mass-occupying soft-tissue neoplasms of peripheral nerves. For specification of a tumor location during planning of operative treatment, additional instrumental methods of research is required. Application of electroneuromyography in diagnostics of this pathology often does not give accurate results, as often patients do not suffer from nervous trunks conductivity abnormality, or, if tumors are located next to the main nervous trunks, only insignificant or moderate abnormality of conductivity comes to light. Application of ray diagnostics methods at peripheral nerves tumors is often limited by possibilities of research techniques. In case of a nervous trunk or soft tissues tumor roentgenography has no importance for diagnostics and it can be carried out only for elimination of bone pathology.
Computer tomography, as well as roentgenography, does not give a required amount of information at this pathology. Magnetic resonance imaging (MRI) is a method of choice in diagnostics of soft-tissue mass-occupying neoplasms, including those connected with large nervous trunks and plexuses. However, if a mass-occupying neoplasm is of a small size and is located with a skew angle to tomographic slices, interpretation of received results can be complicated. Therefore recently appeared method of NLS-research, in our opinion, can become both screening, and the main method of peripheral nerves tumors diagnostics.
We have not found a detailed description of neurofibroma’s NLS-picture in available medical references, at the same time we conducted a research of a group of patients with a similar disease, so we decided to present gathered material. The purpose of our research was evaluation of possibilities of NLS-graphy in diagnostics of peripheral neurofibromatosis.
MATERIAL AND METHODS OF STUDY
Within the period from 2009 till 2012 we studied 15 patients (9 women and 6 men) with palpated soft-tissue neoplasms in various organs of a body, upper and lower extremities, without neurologic semiology, with various degrees of neoplasms morbidity and gradual increase in neoplasms sizes. Patients were aged from 18 till 34. Disease duration was from 2 till 6 years.
NLS-graphy was carried out with device “Metatron”-4025 (IPP, Russia) with the high-frequency generator of 4,9 GHz frequency, unit of continuous spiral scanning allowing to carry out evaluation of ultrastructure of nervous fibers and a genetic apparatus of a nerve cell.
The device was equipped with a professional computer program “Metapathia GR Clinical”, allowing to fulfill, both two-dimensional, and three-dimensional visualization of nerve trunks and surrounding tissues.
In our study we applied NLS-ultramicroscanning mode with spectral-entropic analysis (SEA), allowing to detect spectral similarity of affected nerve tissues to etalon processes “Neurofibromatosis. NF-1” and “NF-2”.
At initial NLS-graphy of nerve trunks, the research was carried out in a three-dimensional mode mainly. It allowed to exclude possibility of small pathological neoplasms un-detection, which is possible at two-dimensional scanning, and to raise accuracy grade of a method.
When changes in a nerve tissue were revealed, we added into research report NLS-scanning in a 4D-Tissue mode with NLS-ultramicroscanning of morphological structures in a zone of interest.
The data obtained during the study was processed by means of statistical program Statistics for Windows (version 7.0)
Results of NLS-research were verified by means of MRI and by histological research of preparations after carrying out of puncture biopsy or operative removal of tumors.
STUDY RESULTS AND DISCUSSION
At preliminary gathering of an anamnesis, it is found out that in 7 of 15 patients there were no manifestations of the disease in their families, and they were the only among close relatives who suffered from this pathology, 4 patients had similar manifestations in relatives maternally, another 4 patients had no such information.
NLS-study of body tissues, upper and lower extremities has shown in all patients hyperchromogenic neoplasms (5-6 points at Fleindler’s scale) of homogeneous structure, with even contour, oval or roundish shape, located in various segments of organs. In 5 patients along with neoplasms of homogeneous structure single neoplasms of moderate chromogeneity (4-5 points) and non-uniform structure were detected. These patients emphasized long period of these tumors existence (3 years and more). In 6 patients neoplasms were located along large nerve trunks, in 9 patients – irrespective of nerve trunks, mainly intramuscularly or hypodermically, in the form of single neoplasms. The quantity of neoplasms was different: from 1 to 7. The sizes varied in a wide range: from 5.0 mm to 4.5cm (measurement of neurofibromas size was done at NLS-ultramicroscanning).
In 10 (66.7%) cases at NLS-ultramicroscanning mode affection of vessels was revealed at the edges of tumors.
Here is a clinical case of NF2NLS-diagnostics.
From an anamnesis of patient P, year of birth – 1980, we found that she suffered pain and swelling for the first time in 2008 in left scapular region for no apparent reason. The patient has come to see a therapist in polyclinic in her community and has been directed to a consultation to a traumatologist-orthopedist. After consultation and inspection in 2009 the patient has been hospitalised in the Clinic named after Priorov, where she was administered to operative removal of a tumour in left scapular region. Histological research of a preparation has confirmed the presence of neurofibroma. Since October 2010 till the present day the patient has complaints about swelling and painful sensations in left scapular region. The patient has been checked-up in 11 traumatology-orthopedic department of the Clinic named after Priorov, where inspection and operative treatment were recommended to her.
At admission to the clinic the general condition of the patient was satisfactory. In the somatic status of the patient no pathology was revealed. The neurologic status: consciousness clear, focused, adequate. No meningeal semiology registterred, pupils OS = OD, photoreaction and corneal reflex are live. Restriction of eyeballs movements is not revealed. Face is symmetric, tongue on an average line. Tendon reflexes from upper extremities are a little more active on the left, muscles tone is without a side difference. No paresis and sensitivity abnormalities.
Visual examination of the patient’s left scapular region in a projection of a trapezoid muscle has detected a small swelling. Palpation of left shoulder girdle detected in soft tissues painful space-occupying process of firm-elastic consistence, not connected to surrounding tissues and partially displaced in a frontback direction. Vascular pattern on a skin in the neoplasm area is not changed, skin temperature is normal. There is a distinct pulsation in peripheral vessels of upper extremities. No sensitive and motion abnormalities in fingers of left upper extremity were revealed.
Under a layer of a skin, hypoderm and front side of a trapezoid muscle NLS-research of left shoulder girdle has revealed a mass-occupying neoplasm of an oval form, with even distinct contour, of high chromogeneity (6 points at Fleindler’s scale), moderately non-uniform structure, sized 3.7 × 2.0 × 2.3 sq. cm. A little laterally from this neoplasm a similar neoplasm of the smaller size – 1.8 × 1.5 × 17 sq.cm. was found. Survey NLS-research of tissues of a left half of neck and area of brachial plexus one more neoplasm (which it was not palpated at clinical survey) was revealed; it was located in immediate proximity from a vascular plexus (common carotid artery and internal jugular), on a NLS-picture it was similar to previous one (oval shape, with the even contour, high chromogeneity (5-6 points at Fleindler’s scale), sizes 1.3 × 1.0 × 0.9 sq. cm. NLS-angiographic research of neoplasms’ periphery has revealed affection of arterial vessels (4-5 points). Regional lymph nodes were moderately chromogenic (3-4 points at Fleindler’s scale), not enlarged. Brachial plexus trunks were located deeper than neoplasms, they had a usual internal structure and uniform thickness.
Applied NLS-research of left shoulder girdle tissues and left half of neck allowed to make a conclusion that the NLS-graphic picture corresponds to NF.
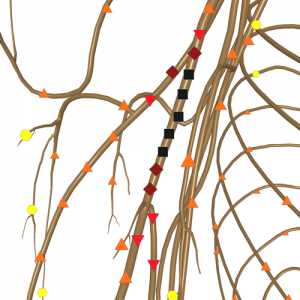
Fig. 1. NLS-gram of neurofibroma in superior third area of a right shoulder.
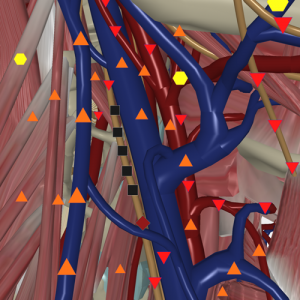
Fig. 2. NLS-gram of neurofibroma, located in the vicinity of common carotid artery and internal jugular vein.
NLS-ultramicroscanning of nerve cell’s genetic apparatus has revealed affection of NF-2 allelic gene.
After NLS-research the patient was administered to surgical removal of neoplasms. During the operation 3 neoplasms were revealed and removed, one of which, located in left shoulder girdle area, grew from a short muscular branch of brachial plexus. Size and external contours of neoplasms almost completely coincided with the NLS-graphic data. On the basis of the operative treatment data “NF” diagnosis was also made.
Histological research has revealed that neoplasms consist of spindle-shaped and roundish cells, with a considerable amount of tissue basophiles. Strom makes a considerable part of tumors and is presented by incoherently located collagenic fibers, plexuses of which are intertwined and located divergently. Affected thin-walled vessels were detected inside tumors. In a preparation tissue basophiles and macrophages are located perivascularly. Immunomorphologic researches have shown that collagen of I and III types prevails in stroma. Positive coloring for S-100 protein, a marker of neurogenic cells, specified neurogenic origin of tumors.
Control NLS-research with SEA in 15 days after operative treatment has revealed no solid neoplasms in areas where tumor were removed. In an area of left shoulder girdle, in a spot where two tumors were removed, a small hematoma in a shape of a cavity with achromogenic content and thin hypechromogenic partitions inside was detected.
On the basis of the patient survey, chromosomal apparatus NLS-research data, operative and histological researches, considering absolute and probable signs NF2, the diagnosis is made: NF2, neurofibromas of brachial plexus branches.

Fig. 3. NLS-ultramicroscanning. NF2 neurofibroma of brachial plexus branches.
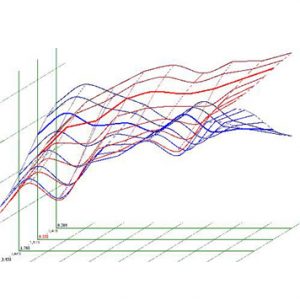
Fig. 4. Spectral-entropic analysis. NF2 neurofibroma.
After applied treatment and discharge from the hospital patient P. has been directed to geneticist’s consultation to interclinical department of medical genetics of Moscow medical academy named after Sechenov.
During our work we have revealed that for the first time NF is manifested in young patients, that corresponds to a data in references, evidencing progressing of the disease in after 20-year-old patients. However the variant with the late development of the disease, which happens in patients above 20, evidences possibility of various types of NF. For example, late beginning happens at NF2 with presence of disease in a family and at NF of 6th type, at which there are no family cases of disease, as it was confirmed during our study.
It is known that distinctive signs of the tumors growing from nerve trunks, are their mobility, displaceability to sides and absence of displacement along a nerve trunk. Our research has also shown absence of neoplasms cohesion with surrounding tissues in patients, tumors were mobile enough, especially those located hypodermically. According to references, all benign tumours are characterised by slow growth that corresponds to data gathered during our research, in which duration of tumors growth was 2 – 6 years.
At NLS-research of patients with NF in 60.0% of cases tumors have been represented by single neoplasms which were located hypodermically and intramuscularly, mainly on extensor surfaces of a body and extremities, and were not connected to main nerve trunks. In 40.0% of cases neurofibromas were located along main nerve trunks and plexuses. Some of small size tumors were detected for by NLS-research for the first time.
Inasmuch the fact that in 9 patients affection of one segment of a body was detected, it was possible to make a preliminary diagnose: segmentary NF (NF5) at which any area of a body, as it is known, is affected. However, as it has been specified earlier, all types of NF, except NF2, are versions of NF1, but in our work we have not received signs of NF1presence at patients. Therefore the given assumption (about presence of NF5), most likely, would be incorrect. At combined type of NF, except peripheral neurofibromas, the basic symptom is the presence of central nerve system tumors, developing most frequently at the age of 20–30 years. In our work we have faced only peripheral NF cases, which affected soft tissues of extremities. However at alternative 4th or 5th type of NF numerous neurofibromas are accompanied by high risk of optic nerve glioma, neurilemmoma or meningioma development. 4 patients from studied group have been subjected to MRI of brain, at which no pathological changes were revealed at the moment of inspection. Other patients were recommended to undergo MRI of a head and, in case of any complaints and clinical manifestations, MRI of a spine for acknowledgement or denial of a central form of pathological process.
Currently the forecast of NF course is uncertain enough, it depends on the form of disease and location of tumors. Frequency of neurofibromas malignization, according to various authors, is from 3% to 15%.
In cases of the inherited disease the risk of a sick child birth is 50%.
According to our data, neurofibromas are located mainly on a border of derma and the upper part subcutaneous fat, and also between subcutaneous fat and muscles, in certain cases – intramuscularly. They can be asymptomatic, be defined by palpation, can be painless or manifested clinically in the form of pain in any segment of a body. At NLS-research – neurofibroma is a space-occupying solid neoplasm of high chromogeneity, of homogeneous structure mainly, various size, oval or roundish (less often) shape.
At the presence of complaints about pain in soft tissues of separate segments of a body or presence of palpated neoplasm, it is necessary to send patients to NLS-research to exclude tumors of peripheral nerves. NLS-research of soft tissues and peripheral nerves can be one of the basic methods of neurofibromas diagnostics in patients of all ages, as it does not require preliminary preparation and anaesthesia.
REFERENCES
1. Inoue Y., Nemoto Y., Tashiro T. et al. Neurofibromatosis type 1 and type 2: review of the central nervous system and related structures // Brain Dev. 1997. V. 19. № 1. P. 1–12.
2. Wishart J.H. Case of tumors in the skull, dura mater, and brain // Edinb. Med. Surg. J. 1822. V.18. P. 393–397.
3. Von Recklinghausen F.D. Ueber die Multiplen Fibrome der Haut und ihre Beziehung zu den Multiplen Neuromen. Berlin: Hirschwald, 1882. S.3–18.
4. Levin O.L. Recklinghausen’s disease: its relation to the endocrine system. Report of an illustrative case // Arch. Derm. Syphilol. 1921. V. 4. № 3. P.303–321.
5. Vassiliev S.А., Zuyev А.А. Neurosurgical aspects of neurofibromatosis of the 2nd type // Neurosurgery. 2008. No 4. p. 69–72.
6. Huson S.M., Harper P.S., Compston D.A. Von Recklinghausen neurofibromatosis. A clinical and population study in south-east Wales // Brain. 1988. V. 111. № 6. P. 1355–1381.
7. Evans D.G., Sainio M., Baser M.E. Neurofibromatosis type 2 // J. Med. Genet. 2000. V. 37. № 12. P.897–904.
8. Gottfried O.N., Viskochil D.H., Fults D.W., Couldwell W.T. Molecular, genetic, and cellular pathogenesis of neurofibromas and surgical implications // Neurosurgery. 2006. V. 58. № 1. P. 1–16.
9. Evans D.G., Huson S.M., Donnai D. et al. A genetic study of type 2 neurofibromatosis in the United Kingdom. I. Prevalence, mutation rate, fitness, and confirmation of maternal transmission effect on severity // J. Med. Genet. 1992. V. 29. № 12. P.841–846.
10. Evans D.G., Huson S.M., Donnai D. et al. A genetic study of type 2 neurofibromatosis in the United Kingdom. II. Guidelines for genetic counselling //J. Med. Genet. 1992. V. 29. № 12. P. 847–852.
11. National Institutes of Health Consensus Development Conference Statement: neurofibromatosis // Neurofibromatosis. 1988. V. 1. № 3. P. 172–178.
12. Tomita T., Radkowski M.A., Gonzalez-Crussi F. et al. Multiple meningiomas in a child // Surg. Neurol. 1988. V. 29. № 2. P. 131–136.
13. Baser M.E., Friedman J.M., Evans D.G. Predictors of survival in neurofibromatosis 2 // Am. J. Hum. Genet. 1999. V. 65. Suppl. 4. P. A61.
14. Huynh D.P., Mautner V., Baser M.E. et al. Immunohistochemical detection of schwannomin and neurofibromin in vestibular schwannomas, ependymomas and meningiomas // J. Neuropathol. Exp. Neurol. 1997. V. 56. № 4. P. 382–390.
15. Zucman Rossi J., Legoix P., Der Sarkissian H. et. al. NF2 gene in neurofibromatosis type 2 patients // Hum. Mol. Genet. 1998. V. 7. № 13. P. 2095–2101.
16. Tsukita S., Yonemura S. Cortical actin organization: lessons from ERM (ezrin/radixin/moesin) proteins // J. Biol. Chem. 1999. V. 274. № 49. P.34507–34510.
17. Zhao Y., Kumar R.A., Baser M.E. et al. Intrafamilial correlation of clinical manifestations in neurofibromatosis 2 (NF2) // Genet. Epidemiol. 2002. V. 23. № 3. P. 245–259.
18. Gronholm M., Sainio M., Zhao F. et al. Homotypic and heterotypic interaction of the neurofibromatosis 2 tumor suppressor protein merlin and the ERM protein ezrin // J. Cell Sci. 1999. V. 112. № 6. P.895–904.
19. Popelyansky Y.U. Diseases of peripheral nerve system: Manual for doctors. М.: Medicine, 1989. 464 p.
20. Belousov А.Е., Tkachenko S.S. Microsurgery in traumatology. L.: Medicine, 1988. 224 p.
21.Verlinsky Y., Rechitsky S., Verlinsky O. et al. Preimplantation diagnosis for neurofibromatosis // Reprod. Biomed. Online. 2002. V. 4. № 3. P. 218–222.
22. Badalyan L.О., Skvortsov I.А. Clinical electroneuromyography. М.: Medicine, 1986. 368 p.
23. Ferner R.E. Neurofibromatosis 1 // Eur. J. Hum. Genet. 2007. V. 15. № 2. P. 131–138.
24. Thomas P.K., King R.H., Chiang T.R. et al. Neurofibromatous neuropathy // Muscle Nerve. 1990. V.13. № 2. P. 93–101.
25. Kuorilehto T., Poyhonen M., Bloigu R. et al. Decreased bone mineral density and content in neurofibromatosis type 1: lowest local values are located in the load carrying parts of the body // Osteoporos. Int. 2005. V. 16. № 8. P. 928–936.
26. Murphey M.D., Smith W.S., Smith S.E. et al. From the archives of the AFIP. Imaging of musculoskeletal neurogenic tumors: radiologic-pathologic correlation // Radiographics. 1999. V. 19. № 5. P.1253–1280.
27. Mautner V.F., Tatagiba M., Lindenau M. et al. Spinal tumors in patients with neurofibromatosis type 2: MR imaging study of frequency, multiplicity, and variety // AJR. 1995. V. 165. № 4. P. 951–955.
28. Fornage B.D. Peripheral nerves of the extremities: imaging with US // Radiology. 1988. V. 167. № 1. P. 179–182.
29. Peer S., Bodner G. High-Resolution Sonography of the Peripheral Nervous System. Berlin: Springer, 2003. 136 p.
30. Martuza R.L., Ojemann R.G. Bilateral acoustic neuromas: clinical aspects, pathogenesis, and treatment // Neurosurgery. 1982. V. 10. № 1. P. 1–12.
31.Ferner R.E., Gutmann D.H. International consensus statement on malignant peripheral nerve sheath tumors in neurofibromatosis // Cancer Res. 2002. V. 62. № 5. P. 1573–1577.
32. Ruttledge M.H., Rouleau G.A. Role of the neurofibromatosis type 2 gene in the development of tumors of the nervous system // Neurosurg. Focus. 2005. V. 19. № 5. P. E6.
33. Viskochil D., Carey J.C. Alternate and related forms of the neurofibromatosis // The Neurofibromatoses / Ed. by Huson S.M., Hughes R.A. London: Chapman & Hall, 2007. P. 445–474.
34. Nesterov V. I. “Computer nonlinear diagnostics” // Collection of scientific works of the Institute of Practical Psychophysics “Actual problems of NLS-diagnostics”. Volume I. М: Katalog, 2006, p. 5-6.
35. Nesterov V.I. “3D NLS diagnostics. Prospects of development” Collection of scientific works of the Institute of Practical Psychophysics “NLS-technologies in medicine – prospects of development”. Volume III. М: Katalog, 2010, p. 5-8.
