G. Muller, A. Rosenberg
Betanien Clinic, Frankfurt on the Main
Introduction
New medical technologies have been developing very quickly in the last decades. A significant success was achieved in treatment of oncological and oncohematological diseases. Development of transplantology increases chances of oncologic patients for recovery. However application of cytostatic and immune suppressing medications, ensuring functioning of transplantates, leads to severe decreasing of immunity and appearance of complications in a form of opportunistic infections. Besides, group of infections development risk includes patients suffering from acquired immune deficiency syndrome (AIDS), complications after abdominal surgical interventions, major severe burns, and premature newborns or newborns subjected to aggressive medical therapy within the first days of life (parenteral feeding and massive antibacterial therapy). Among contributive risk factors of invasive mycoses development are intake of antibiotic with a wide spectrum for more than two weeks, total intravenous nutrition, continuous artificial lung ventilation, shock, preceding mycotic infections.
Results of 8124 autopsies show that incidence of mycotic infections in clinics of Frankfurt on the Main has increased from 2.2% in 1978 to 5.3% in 2004. This increase happened mainly due to aspergillus infection, incidence of which has increased 10 times within this period of time.
A peculiarity of aspergillus infection course is a variety of its clinical manifestations. Therapists single out invasive and non-invasive aspergillosis.
Invasive pulmonary aspergilliosis (IPA) is the most severe form of the disease, when dissemination of the process into other organs (CNS, parenchymatous organs of abdominal cavity) is possible. Often the first symptom of invasive mycotic infection is a fever, refractory to broad-spectrum antibiotics. Absence of a result at treatment with antibacterial preparations at clinical picture of acute pneumonia in patients with expressed immune suppression must be regarded as a possibility of IPA development. When such clinical manifestations are registered diagnostic maneuvers must be fulfilled. Speed and intensity of IPA manifestations depend on degree of immune suppression. IPA signs reveal themselves distinctly after granulocytopaenia, Sometimes IPA diagnosis may be made basing on results of a biopsy only, but a risk of haemorrhagic complications in patients with hemoblastoses may be one of barriers for biopsy.
Materials and methods
Altogether 55 patients suffering from IPA were investigated. The diagnosis was made on the basis of combined clinical, immunological, histological, mycological studies of patients subjected to a hospital treatment in mycology department of Betanien clinic and outpatiently.
Diagnoses were made using criteria of invasive mycoses diagnosing, developed by the European institution of cancer study and treatment and Mycology research group of the Institute of Allergy and Infectious Diseases of USA.
Clinical methods of investigations included examination by a therapist, clinical and biochemical blood tests, fiber-optic bronchoscopy, study of external respiration function. Microbiological study was carried out in accordance with standard practice. To reveal supersensitiveness of an organism to possible allergens, the researchers applied a method of skin testing and revealing of specific IgE in blood serum. Allergological testing was carried out in allergology room of mycology department.
To fulfill mycological examination of a phlegm and liquid from bronchi, phlegm was gathered into a sterile container after cleaning of mouth cavity (tooth brushing, gargling with soda liquor), liquid from bronchi was gathered during bronchoscopic investigation.
To carry out histological research the authors used paraffin and frozen section, colored with haematoxylin and eosin, azure II-eosin, Gram-Weigert method, PAS-response, Grocott-Gomori method.
Precipitating antibodies to Aspergillus spp. antigens were defined applying enzyme multiplied immunoassay (EMI). A part of patients was subjected to precipitation reaction.
Total IgE and specific IgE to A.fumigatus was found using methods of radioimmunosorbent test in a nuclear medicine laboratory and enzyme multiplied immunoassay in a laboratory of allergens and allergy diagnostics. Measuring of total IgE was done in kU/l (thousands of international units in a litre, 1 unit = 2.4 ng).
А.fumigatus antigen was defined by latex particle agglutination mathod by Pastorex company.
Diagnostic investigation of patients included roentgenography and computed non-linear study (NLS) of a thorax. The goal of NLS-graphy of a thorax was to reveal and locate changed pulmonary parenchyma, detecting of symptoms typical for mycotic affection, and revealing of NLS-picture dependence on clinical symptoms and laboratory research data.
Thorax investigation was carried out using a device manufactured by Siemens Company (Germany) in two projections (frontal and lateral), supported by tomograms. NLS-graphy was carried out using “Metatron”-4025 system (IPP, Russia) equipped with high-frequency generator of 4.9 GHz, unit of continuous spiral scanning and professional software “Metapathia GR Clinical”, which allowed to carry out three-dimensional visualization of lungs.
During the research we used NLS-ultramicroscanning mode with spectral-entropic analysis (SEA), allowing to evaluate spectral similarity of affected lung tissues to “Aspergillus fumigatus” etalon. During the initial fulfillment of NLS-graphy of thorax organs, the examination was dome in three-dimensional mode mainly.
Differing from two-dimensional scanning it allowed to exclude a possibility of small pathological lesions (nidi, cavities, bronchiectasis, etc.) missing, and to increase a resolution along longitudinal axis of scanning in order to check lateral structures, located perpendicularly or at an angle to NLS-gram plane.
When pathological changes were found, the research was extended with NLS-scanning in 4D Tissue mode with NLS-ultramicroscanning of morphological structures in a researched area. Some patients were subjected to repeated NLS-studies in order to evaluate dynamics of changes, revealing of complications and monitoring of therapeutic interventions. At assumption of mycotic process dissemination, we carried out NLS-ultramicroscanning and SEA of other anatomic regions (abdominal cavity, brain, paranasal sinuses).
Data acquired during the study was processed at a PC IntelPentium 166 MMX using software system Statistica for Windows (version 5.11).
Results and discussion
Altogether 55 patients suffering from IPA were investigated. In 54 patients IPA was developing against the background of significantly decreased immunity (neutropaenia < 0.1 x 1 mld/l).
The main category of patients with IPA consisted of patients from oncohematology department (52 patients). Another 2 patients suffered from multiple bronchiectasis and AIDS and were continuously taking glucocorticoid preparations.
In one patient IPA developed when he was completely healthy. However it was known that this patients worked at hay storage, where risk of Aspergillus infestation is increased. Age of all studied patients varied from 7 to 63 (on the average 31.9 ± 2.21 years old). Men prevailed in this group of investigated patients – 34 (61.8%).
Revealing of A.fumigatus antigen in blood was carried out in all patients. A positive result was registered in 82% of cases. Cultural investigation of a phlegm and bronchoalveolar lavage was fulfilled in 69%, growth of A.fumigatus was registered in 24% and 40% correspondingly. At microscopic evaluation of a phlegm and bronchial liquid mycelium was found in 12% and 20% of cases correspondingly.
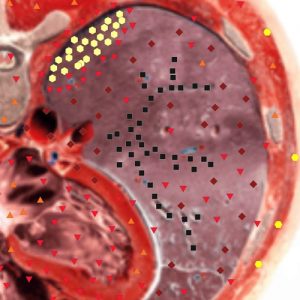
In 98.6% of patients IPA was diagnosed with spectral-entropic analysis. In affection nidi a high spectral similarity to “Aspergillus fumigatus” etalon (D<0.425) was found. At the early stages of IPA development high body temperature, more than 38°С, refractory to antibiotics, was registered in 54 (98%) cases, couching – in 34 (62%), pneumorrhagia – in 13 (24%). 13 (34%) patients complained about pain in thoracic region. Dissemination of the process, revealed by SEA, was registered in 3 (5%) patients, at the same time in all of them cerebral affection was diagnosed. During the study 14 (26%) patients died. In one case we registered self-recovery of the patient, in which IPA developed against the background of normal immunity.
At the early stage of IPA development (fever) radiographic examination has revealed interstitial changes in 22% of patients. In 19% of patients nidi were registered. Roentgenograms showed absence of any changes in 75% of studied patients. During studies in dynamics repeated roentgenograms of a thorax at progressing process revealed multiple nidi, foci and areas of lung tissue infiltration in 40%, 47% and 25% correspondingly. Lungs affection was ambilateral in 75% of cases. In 2 (3.6%) patients on 3-4 week IPA pathognomonic symptom was detected.
At the same time detecting of this symptom concurred with finishing of agranulemia period. It should be noted that even at application of corresponding antimycotic therapy and positive clinical dynamics, changes in lungs significantly increased after neutropaenia period was over. This condition was registered in 15 (27%) of patients. After continuous therapeutic interventions we detected decreasing of amount and intensity of changes in lungs.
NLS-semiotics of IPA varied. Table 1 shows data about various types of changes in lungs, registered in patients with neutropaenia.
He most frequently registered change of pulmonary parenchyma at IPA were nidi and foci of hyperchromogeneity (5-6 points at Fleindler’s scale) of pulmonary tissue – 75%.
Alveolar infiltration was detected in 1/3 of patients approximately.
One of the most serious complications of IPA is infarction pneumonia-pneumonia; it was registered by NLS-graphy in 7 (13%) patients. At the same time we detected areas of hyperchromogeneity of pulmonary tissue of conical form, adjoining pleura with broad side. With the same frequency hydrothorax development was revealed.
It should be notes that revealed nidi, foci and pulmonary tissue infiltration areas in majority of cases had subpleural location.
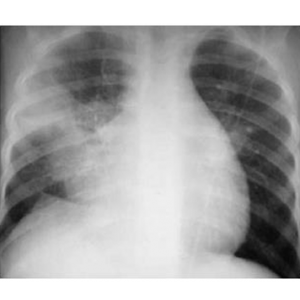
Pic.2. Patient S., 10 years old. AML. IPA. Survey radiograph of a thorax. Massive infiltrative changes in medium areas of a right lung of heterogeneous character with uneven contours. Decreasing of a right lung volume, dome of a right half of a diaphragm is lifted upwards.

Pic.1. Patient Т., 14 years old. Acute myelogenous leukemia (AML). IPA. Survey radiograph of a thorax. In paramediastinal regions of both lungs multiple infiltration nidi with uneven contours are detected.
Besides, approximately in a half o cases NLS revealed a connection of foci with vessels. Radiographic examination never revealed such symptom.
We have note a connection between NLS- symptom complex and duration of the disease. However data acquired at roentgenography and NLS-study had certain differences. To show the most demonstrational distribution of symptoms in time we have chosen 3 time periods since the moment of the first clinical symptomatic appearance: 1st – 4th day, 4th – 8th day, 8th – 20th day.
Table 1. Parameters of NLS-study and roentgenography in diagnostics of lungs mycotic affection
|
Parameter, % |
IPA |
||
|
NLS |
p |
roentgenography |
|
|
Sensitivity Specificity Predictive value: positive negative Diagnostic accuracy |
85 75
75 86
80 |
– –
– –
<0,05 |
44 78
75 48
58 |
The earliest signs of IPA were nidal and interstitial hyperchromogenic changes of tissues, revealed by NLS-study in 75% and 67% of cases correspondingly. Roentgenography turned out to be less informative during the initial stage. Frequency of nidal and interstitial changes revealing according to roentgenography data was statistically reliably lesser – 19% and 42% correspondingly. Foci of alveolar infiltration were revealed in a significantly lesser percentage of cases according to both methods.
Nidal changes of pulmonary tissue during the second period of time (4th – 8th day) were revealed less frequently than during the first period of time. Frequency of interstitial changes areas revealing was also lesser. Foci had different shapes, more often roundish, homogeneous structure, were of subpleural location and had a connection with vessels.
The third period of time (8th – 20th day) was marked by even less amount of changes revealed according to both methods.
During the third period of time we registered IPA pathognomonic symptom – air crescent sign, represented by moderately chromogenic cavity with roundish solid content. The content was separated from a wall by thin crescent achromogenic layer of air, resembling crescent moon. The sign was revealed in 9% by NLS-study and in 3.6% by roentgenography.
In one patients we diagnosed a pneumothorax.
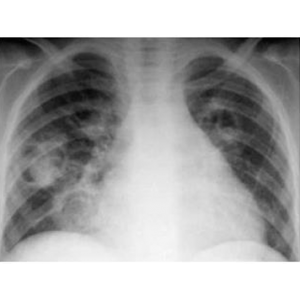
Pic.3. Patient F., 7 years old. AML. IPA. Survey radiograph of a thorax. In both lungs we detected roundish thin-wall cavitary lesions with a solid content, adjoining lower walls of cavities and forming a crescent symptom.
In 87 % of cases NLS-study has revealed a pathological changes in both lungs.
First of all IPA was diagnosed in patients with significant decreasing of immunity (neutropaenia < 0.1 x 1 mld/l). In all these patients we detected high spectral similarity with “Aspergillus fumigatus” etalon (D= 0.108 ± 0.035), revealed by spectral-entropic analysis.
Complaints of IPA patients were nonspecific and included a fever resistant to antibacterial therapy.
The main antibody-mediated method of IPA diagnostics was detection of Aspergillus mycete. Also we used data of mycological examination of a phlegm and bronchoalveolar lavage.
Speaking of hardware investigations, NLS-graphy turned out to be more informative in comparison with traditional roentgenography; NLS helped to reveal pathological changes in a pulmonary tissue more frequently (p < 0.05). Cases with ambilateral lung affection prevailed.
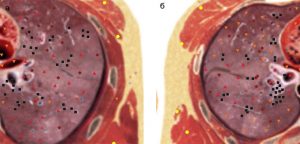
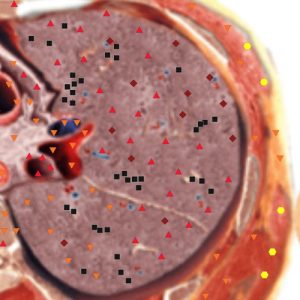
Pic 4. Patient А. 21 years old. AML. IPA. NLS-grams. In S VI of a right lung (а) and S I+II,IV of a left lung (б) hyperchromogenic nidi with uneven contours were revealed.
NLS-semiotica of IPA included nidal and interstitial hyperchromogenic changes, revealed most frequently at the early stages of the disease (1st – 4th day since the moment of clinical manifestations).
On 5th – 7th day we mainly registered foci and areas of alveolar infiltration, which evidenced progressing of the process. We should note subpleural localization of nidal and interstitial changes mainly, and revealed by NLS-study connection of nidi and infiltration foci with vessels.
During the later period, starting from the 8th day since clinical manifestations, changes were polymorphous: we could see isochromogenic nidi, foci and infiltration areas, in rare cases – interstitial changes of pulmonary tissue. Only during the third period of IPA we registered air crescent symptom. Revealing of this symptom was a positive sign and it evidenced resolution of pathological changes.
Pic 6. Patient G. 22 years old. AML. IPA. Computed NLS-gram at a level of a heart. In SX of a left lung a zone of pulmonary, tissue affection where crescent-like air gap is seen, was found.
Pic 5. Patient Т. 14 years old. AML. IPA. Computed NLS-gram. In a right lung hyperchromogenic foci of interstitial infiltration linked to vessels were found.
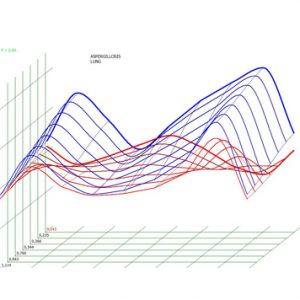
Pic 8. Spectral-entropic analysis. Pulmonary aspergilliosis (D=0,143).

Pic 7. Patient Kh. 56 years old. Lymphosarcoma. IPA. NLS-ultramicroscanning. Affection of pulmonary tissue, as a manifestation of infarction-pneumonia at progressing IPA is detected.
Appearance of infiltration areas of conical form, adjoining pleura with broad side, evidenced development of infarction-pneumonia, which was one of IPA manifestations as a result of vessel wall infiltration and its lumen obstruction with filaments. A sign of a negative prognosis was fine-focal hypechromogenic dissemination, which was detected in lungs of patients with aspergillosis generalization. In all three cases a brain was affected because of generalization; changes in a brain were confirmed by NLS and MRI data, succeeded by lethal outcome.
It should be noted that during examination of IPA patients NLS-graphy was more informative in comparison with traditional radiographic examination (see Table 1).
Conclusion
1. NLS-graphy is more informative method in diagnostics of invasive pulmonary mycoses in comparison with roentgenography. Its sensitivity is 86%, specificity – 75% and diagnostic accuracy – 80% (67.2-90.3) (p < 0.05).
2. X-ray pattern depends on duration of the process at IPA. In the beginning of the process (1st – 3rd day) the most frequently revealed sign is nidal and interstitial changes of lungs (75%). 4th – 7th days are characterized by prevalence of roundish induration of pulmonary tissue (75%), halo symptom is revealed (40%). After 8th day nidal and interstitial changes are revealed less frequently, air crescent symptom may be registered (9%).
References
1. Fridkin S.K., Jarvis W.R. Epidemiology of nosocomial fungal infection // Clin. Microbiol. Rev. 1996. V. 9. N4. P.499–511.
2. Groll A.H., Shah P.M., Mentzel C. et al. Trends in the postmortem epidemiology of invasive fungal infections at a university hospital // J. Infect. 1996. V. 33. N1. P. 23–32.
3. Denning D.W. Invasive aspergillosis // Clin. Infect. Dis. 1998. V. 26. P. 781–805.
4. Rosenberg A.S., Armstrong D. Aspergillus infection in the cancer patients // Infect. Med. 1993. V. 10. N8. P. 10–40.
5. Ascioglu S., Rex J.H., Pauw B. et al. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplant: an international consensus // Clin. Infect. Dis. 2002. V. 34. P. 7–14.
6. Makarova S.N. NLS-diagnostics of lung abscess // Collection of scientific works of the Institute of Practical Psychophysics “Actual aspects of NLS-diagnostics”. Tome I. М.: Katalog, 2006, p. 27-29
