V.I. Nesterov, A.Y, Tsukanov, V.N. Nikitin
The Institute of Practical Psychophysics, Omsk
Department of surgical pathologies of Omsk state medical academy
Introduction
At the present moment non-linear diagnostics (NLS) is one of the most promising methods of visualization in many fields of practical medicine. One of the most significant fields is NLS-diagnostics of lung abscesses, however medical literature pays insufficient attention to this issue.
Traditionally diagnostics of purulent-destructive diseases of lungs is fulfilled by roentgenologic study, which is still a golden standard in detection of this pathology, but has a number of limitations. The most important among them, besides radiation exposure of a patient and a therapist – is images summation effect and impossibility to differentiate liquid and tissue structures at the same density of a shade. NLS has no such disadvantages and it provides conceptually new possibilities in visualization of pathological changes by rendering of their three-dimensional image with high spatial and dynamic resolution capability.
Computed tomography creates three-dimensional image with high resolution also, but CT is less available that NLS-study, besides, a special attention must be paid to a specific character of contingent of patients with purulent-destructive diseases of lungs and clinical picture of a disease. That is why in practice lung abscess is diagnosed on the basis of clinical symptoms and thorax x-ray data, however with these methods it is not always possible to identify a nature of a nodular shadow in a lung. Application of NLS allows to get additional and sometimes decisive information about a pathology, but in this case a therapist must know NLS semiotics of lung abscess.
So the objective of this work is to study a picture of lung abscesses and evaluate possibilities of NLS of thorax in diagnostics of purulent-destructive process in lungs.
Material and methods
In medical sanitary station No.1 of Omsk we carried out NLS of thorax of 145 patients in 2009-2012. The research was made with use of Metatron-4025 device (IPP, Omsk) with high-frequency sensor of 4.9 GHz and a method developed by the medical station. At visualization of a pathological formation we identified location, size and chromogeneity; and using spectral-entropic analysis (SEA) – morphological structure. We studied changing of NLS-picture in dynamics. Results of NLS were verified by data acquired with clinicoroentgenologic inspection, abscesses puncture with following microbiological and cytological analysis, surgical interventions (in general – thoracoabscessotomy).
Results and discussion
In accordance with introduced syndrome-related approach to ultrasound diagnostics of thoracic organs, lung abscess in included into a syndrome of parietal formation. The common NLS sign of this syndrome is a presence of parietal pathological nidus.
Topical diagnostics was carried out in accordance with generally accepted projection of lobes and segments of a lung to a thorax surface. S6 and S10 of inferior lobe and S2 of superior lobe ware affected. The majority of abscesses were of oval shape with a short axis perpendicular to a thoracic wall, at the same time long axis was both vertical and horizontal. Size varied from 3 to 13 cm, but in general it was 5-8 cm.
NLS semiotics of lung abscesses is diverse and depends on a content of its cavity and a condition of surrounding tissues. The main diagnostic criteria are structure and contours. NLS structure helps to identify liquid or gaseous body of content, and when they are combined – prevalence of one of the components and character of its spreading in purulent cavity, and on the basis of this information to evaluate efficiency of destruction nidus draining by bronchi and make a conclusion about purulent or gangrenous type of a disease. NLS picture of contours allows to judge about duration of existence and degree of delimitation of purulent cavity from surrounding lung, condition of surrounding parenchyma and possible chronisation of a process.
For the first time we have offered an original NLS classification of lung abscesses, basing on evaluation of destruction nidus structure, namely on quantitative ratio of hyperchromogenic purulent exudate and achromogenic air inclusions and in a pattern of their spatial location in a cavity. Depending on efficiency of abscess spontaneous draining by bronchi we have singled out 4 NLS variants, which represent consecutive stages of purulent-destructive process development in a lung:
1. Blocked abscess.
2. An abscess with insufficient spontaneous draining.
3. An abscess with sufficient spontaneous draining.
4. An abscess with air cavity.
Blocked abscess represents early closed stage of lung destruction with formation of purulent cavity, surrounded by lung parenchyma and not linked with bronchial tree. On an NLS-image it looked like a roundish nidus, frequently with homogeneous NLS structure, presented by liquid hypechromogenic content (6 points at Fleidler’s scale) with isochromogenic suspended matter (purulent detritus), but without achromogenic signals of air. Suspended matter was various in chromogeneity, density and character of distribution in a cavity of destruction. As a rule it was close-bodied, quaggy and occupied the whole abscess, not causing any diagnostic difficulties.
With equally high density thick purulent content imitated moderately chromogenic tumorous tissue, and because of that differential diagnostics with lung cancer was needed. Heterogeneous suspended matter could form local aggregates of lesser chromogeneity, imitating sequesters. SEA grants help in diagnostics.
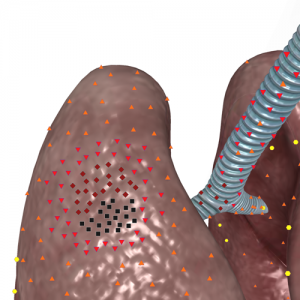
Pic. 1. 3D NLS-graphy of lung. Blocked acute purulent abscess with homogeneous structure, represented by: – isochromogenic content with close-bodied suspended matter; – hyperchromogenic content with dense suspended matter, imitating peripheral cancer.
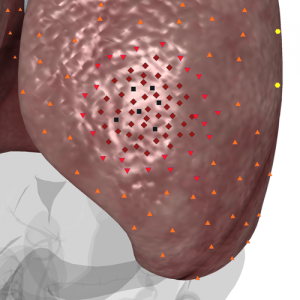
Pic. 2. 3D NLS-graphy of lung. Acute purulent abscess intracavitary with metastases. Seminoma in form of oval chromogenic formations of constant shape.
A cavity had no visible wall and was limited by lung parenchyma itself, which, at preserved airiness, was located as a hypochromogenic strip of various width with uneven outer border; at loss of airiness – as a slightly chromogenic tissue around destruction nidus.
Burst of a purulent exudate into a bronchial tree meant beginning of open stage of an abscess with presence of one or several draining bronchi, through which air went to a cavity of destruction and liquid content was removed. This stage is characterized by strictly heterogeneous structure of a nidus due to appearance of multiple achromogenic signals against the background of hypechromogenic content.
Depending on efficiency of a purulent cavity clearing through bronchi we singled out abscesses with insufficient spontaneous draining and with free spontaneous draining. Efficiency of draining was evaluated according to quantitative ration of liquid and gaseous content and character of air distribution in a cavity of destruction. The stages are dynamic and can transform one into another depending on evacuating function of bronchi, severity of perifocal inflammation, activity of purulent-destructive process and character of cavity’s borders.
At insufficient spontaneous draining we located lesser single and multiple achromogenic signals in an abscess, which were diffusely distributed with a background of significantly prevailing liquid content. In certain cases they accumulated in one of regions in form of larger achromogenic inclusions. At long-lasting large cavity certain amount of air accumulated in its superior part, forming air inclusion. In almost 1/3 of patients with blocked abscesses and insufficient spontaneous draining of purulent cavity, we registered increasing of chromogeneity of a suspended matter in parietal areas, imitating a wall.
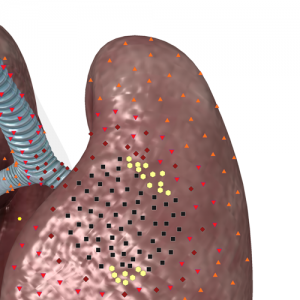
Pic. 3. 3D NLS-graphy of lung. Large acute purulent abscess with insufficient spontaneous draining. Dense suspended matter has pseudo-solid structure, against its background we achromogenic signal from air bubble at external wall. Another air bubble can be seen closer to lower border of a cavity.
At free spontaneous draining the main volume of exudate was already removed through bronchi, and entered air in sufficient amounts formed large bubbles in a structure of exudate and was accumulated in superior parts of an abscess. This stage was characterized by division of a content into superior gaseous layer and inferior liquid layer. Free air in a cavity of an abscess looked like continuous achromogenic line. At major stickiness of purulent exudate, instead of continuous line we found several achromogenic nidi, located step-by-step next to each other. Liquid content occupied inferior part of an abscess, it contained achromogenic air inclusions, spread diffusely or with a layer of air bubbles.
Hypochromogenic border of a lung around clearly separated abscesses had clear and even contour. At vague bordering a contour of a purulent cavity was very uneven and serrated. Hypochromogenic line disappeared at the level of bordering hyperchromogenic area, corresponding to areas of inflamed infiltration into lung tissue. In these areas a border between exudate and lung parenchyma was vague.
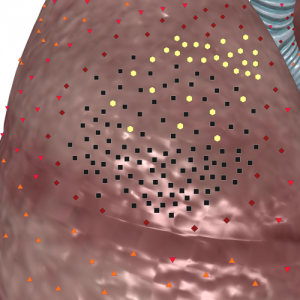
Pic. 4. 3D NLS-graphy of lung. Acute purulent abscess with free spontaneous draining. Achromogenic nonlinear air signal in upper half of an abscess;
Step-like location of hyperchromogenic signals in lower part and interlayer with multiple small air bubbles at high density of purulent exudate.
An abscess inside pneumonic infiltrate or obstructive atelectasis had no achromogenic areal around itself due to weak chromogeneity of surrounding pulmonary tissue. A contour of a destruction nidus was traced along border of hyperchromogenic content of an abscess and hypochromogenic lung tissue. The main difference of an abscess with a background of pneumonia was clear achromogenic air component in a liquid content. Burst of purulent exudate into bronchi happens quite early at relatively small cavity of destruction. In obstructive atelectasis even large cavities of destruction were filled with liquid content without achromogenic inclusions, because air could not penetrate there due to complete obstruction of a bronchus by tumor.
In accordance with pathomorphological picture of an abscess, its walls are formed not earlier than V stage of a disease, so they cannot be visualized at early stages. Before this a nidus of destruction is limited by lung tissue itself with necrotic and fibrinous changes on its surface. A wall along the whole perimeter of a cavity was registered at chronic and continuous abscesses, its NLS picture had a decisive meaning in differential diagnostics with cavitary form of lung cancer. SEA results were the most important diagnostic criteria.
At NLS image abscess wall was represented as thin (less than 5-6 mm) moderately chromogenic frame of even thickness, separating purulent content from surrounding lung tissue. Its external contour was more uneven and jagged than internal, visualization accuracy of which depended on chromogeneity of content. Many times we saw increased chromogeneity and density of suspended matter in parietal parts of destruction cavity in comparison with central parts. It resulted in visual thickening of true border between liquid exudate and a wall.
We carried out a detailed study of NLS picture of gangrenous abscesses in order to optimize treatment tactics and found that along with above mentioned signs, they had certain peculiarities of NLS-picture. The most typical symptom were sequesters of necrotic lung tissue. They represented fragments of necrotic lung, rejected due to purulent-destructive process and separately located in a cavity of destruction. At NLS image sequesters looked like moderately chromogenic areas of irregular shape, with uneven and sometimes indistinct contours located inside abscess cavity and to related to surrounding lung tissue. They were characterized by moderate chromogeneity and stood out against a background of hyperchromogenic content. Sequesters were sized, as a rule, less than 2cm, but sometimes larger fragments were detected.
Macroscopic basis of an early stage was a large cavity of destruction with insufficient spontaneous draining, indistinctly separated from surrounding lung tissue and filled with purulent exudate and sequesters. On NLS image it was comparable with a large abscess of heterogeneous structure due to diffuse distribution of lesser achromogenic air signals against the background of prevailing moderately chromogenic content with coarse suspended matter and possible hypochromogenic sequesters. Irregular shape and uneven contours of a nidus, indistinct in spots inflammatory infiltration of surrounding lung were typical. Destruction cavity is limited by pulmobary tissue without chromogenic walls.
The most frequent complication of lung abscess was formation of bronchopleural fistula with development of empyema and pyopneumothorax, in certain cases accompanied by thoracic wall phlegmon and thoracal fistula. In one patient, who failed to find medical attention in time to treat an abscess of medium lobe of a right lung, we detected gigantic subdiaphragmatic abscess that developed as a result of cupula of diaphragm destruction with a background of pleural empyema.
The most favorable outcome of lung abscess is a complete collapse of a cavity with development of nidal fibrosis. As a stage of cicatrizing cavity an abscess looked like a small (less than 4 cm) parietal nidus with typical irregular or star-like shape, uneven serrate contour and heterogeneous structure because of short achromogenic air signals with prevailing hyperchromogenic background. At complete cicatrization of a cavity on its place we detected remaining small subpleural hypochromogenic area of irregular-shaped sclerosis, with uneven contours and significantly decreased or absent respiratory mobility. Less favorable outcome is formation of residual achromogenic air cavity similar to false cyst.
Conclusion
NLS of thorax is highly informative method of lung abscesses diagnostics, allowing to identify a stage and character of suppurant process, evaluate spontaneous draining of destruction cavity and rate of its separation from pulmonary tissue. At dynamic monitoring this method allows to evaluate efficiency of conservative treatment and define indications for surgical intervention, and to identify possible complication in proper time. NLS of thorax should be more extensively introduced into clinical practice of specialized departments of thoracic surgery, therapeutic and surgical in-patient hospitals.
References
1. Makarova S.N. NLS-diagnostics of lung abscesses. // Collection of scientific works of the Institute of Practical Psychophysics “Actual aspects of NLS-diagnostics”. Volume I. М.: Katalog, 2006, p. 27-29
2. 1. Makarova S.N. NLS and x-ray methods in diagnostics of acute purulent lung abscesses. // 3D computed NLS-gpahy: collection of works/Edited by V.I. Nesterov. – М.: OJSC Publishing house Prospect, 2012, p.30-31
3. Nesterova V.I., Kuznetsova Т.G., Ogluzdina N.L. NLS-diagnostics of diffuse infiltrative diseases of lungs. // Collection of scientific works of the Institute of Practical Psychophysics “Actual aspects of NLS-diagnostics”. Volume I. М.: Katalog, 2006, p. 34-39
4. Nesterov V.I. 3D NLS diagnostics. Prospects of development. // Collection of scientific works of the Institute of Practical Psychophysics “NLS-technologies in medicine – prospects of development. Volume III. М.: Katalog, 2010, p. 5-8
