A.M.Shmerkovich, K.S.Kogan
Moscow scientific-research oncological institute named after Gertsen P.A.
This article explains the possibilities of 3D NLS-graphy in full-scale study of urinary bladder tumors. 365 patients suffering from malignant tumoral affection of urinary bladder were examined. 317 patients (86.8%) suffered from bladder cancer, 4 patients (1.1%) suffered from sarcoma, 6 patients (1.6%) suffered from tumor deposits of another primary site, 2 patients (0.5%) suffered from malignant non-Hodgkins lymphoma with bladder affection, 36 patients (9.9%) had tumor ingrowths into bladder wall from adjacent organs. Possibilities of the method in primary and differential diagnostics and also in detection of local prevalence of urinary bladder tumors depending on their localization are demonstrated in the given article. There is also a description of the difficulties when performing NLS-diagnostics of urinary bladder tumors.
INTRODUCTION
Malignant urinary bladder tumors fill 8th position in male and 18th position in female patients within the structure of oncological diseases. Urinary bladder tumor is in the 4th position among oncourological diseases according to the absolute rate of growth (the first three positions are: prostate cancer, renal cancer and testicular cancer). The multiplicity of rudiments and frequent recuring is characteristic for the tumors of urinary bladder.
In all the countries in majority of cases (90-95%) the tumors of urinary bladder are morphologically transient cell carcinomas; the rest of cases relate to squamous cell cancer and adenocarcinoma. Non-epithelial tumors consist less than 1%.
The main and the most reliable method of urinary bladder cancer diagnostics in clinical practice is still cystoscopic examination with gathering of cytological or histological material. But this method does not allow estimation of tumor invasion depth into bladder wall. The depth of invasion is one of the essential factors when choosing surgical treatment: transurethral resection is not possible in case of affection of wall’s muscular layer (category T2). In case of invasion of perivesical cellular tissue and tumor spread to the adjacent organs (T3-T4) the risk of regional lymphatic glands affection increases: it consists 30% at T2 stage and it reaches 65% at stage T4.
Computer tomography, magnetic resonance tomography and transurethral ultrasonic examination are mainly used over the last years as corrective diagnostics methods to determine the depth of urinary bladder tumor invasion. According to the information provided by Nesterova V. and others the recent method of 3D NLS-research may become crucial both when specifying the prevalence rate of bladder cancer and when performing case monitoring. Such advantages of the method as availability, painlessness and absence of radiation exposure allow performing multiple researches when carrying out case monitoring.
Goal of the given article is to study 3D NLS-research possibilities in primary and corrective diagnostics of malignant urinary bladder tumors, examination of complications which develop during NLS-research of urinary bladder and also systematization, correction and supplementation of NLS-semiotics of urinary bladder tumors.
MATERIAL AND METHODS OF THE STUDY
Full-scale 3D NLS-research of 365 patients (aged 26 – 83) with malignant tumoral affection of urinary bladder was performed in the Institute named after Gertsen P.A. 317 patients (86.8%) suffered from bladder cancer, 4 patients (1.1%) had sarcoma, 6 patients (1.6%) suffered from tumor deposits of another primary site, 2 patients (0.5%) had malignant non-Hodgkins lymphoma with bladder affection, 36 patients (9.9%) had tumor ingrowths into bladder wall from the adjacent organs. Male patients consisted the majority – 273 patients (74.8%) and 92 female patients (25.2%).
All patients were examined using 3D NLS-research of urinary bladder. In all cases the microscanning of urinary bladder wall with spectral-entropy analysis of tissue structures was performed to provide differential diagnostics of various cancer types. 3D NLS-research was performed using «Metatron»-4025 system (IPP, Russia) with 4.9 GHz frequency sensor.
All patients were operated on not later than 2 weeks after performance of NLS-research, the data of morphological research were compared with the results of NLS-ultramicroscanning with spectral-entropy analysis.
We have carried out NLS-ultramicroscopic research of 28 patients with no urinary bladder pathologies to examine NLS-ultramicroscopic features of healthy urinary bladder wall.
RESULTS AND DISCUSSION
1. Ultramicro-NLS-semiotics of urinary bladder tumors. Difficulties of NLS-diagnostics of urinary bladder tumors
We have developed ultramicro-NLS-semiotics of healthy urinary bladder wall and urinary bladder wall with tumoral affection. Healthy urinary bladder wall has 2.5-8.0 mm. in thickness (depending on its filling). In majority of cases it is possible to visualize 3 layers of bladder wall:
1) inner layer corresponds to mucous membrane with submucous layer; in its normal state – moderate hypochromogenic (2-3 points according to Fleindler’s scale);
2) middle layer corresponds to muscular layer; in its normal state – hypochromogenic (2 points according to Fleindler’s scale);
3) outer layer corresponds to adventitious membrane; in its normal state – a-hypochromogenic (1-2 points according to Fleindler’s scale);
Most commonly urinary bladder cancer in 3D NLS-microscopic image has an appearance of exophytic formation of high hyperchromogenecy (5-6 points according to Fleindler’s scale) of round or irregular-shape with uneven surface. In case of absence of infiltrating growth the line between tumor bottom and urinary bladder wall is sharply defined, even and hypochromogenic (1-2 points). In case of infiltration the line between tumor bottom and urinary bladder wall firstly becomes uneven, obscure then there appear tumor structures in the wall’s depth. In this case wall layers stop differentiating. If the tumor grows into the whole wall’s depth then the outer contour of the wall becomes uneven, sometimes obscure.

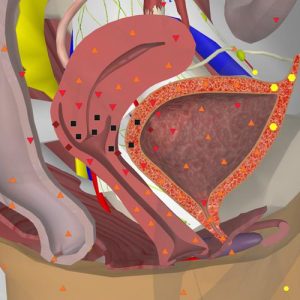
Pic. 1. 3D NLS-graphy. Bladder cancer in urinary triangle area. Tumor grows into prostate gland
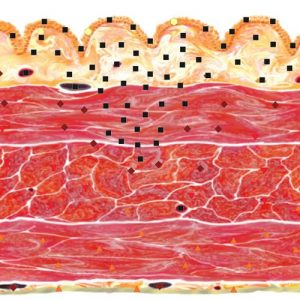
Pic. 2. NLS-ultramicroscanning of urinary bladder wall. Urinary bladder cancer. Onset of invasion of muscular layer.
Tumor with an endophytic component in invasion area is most frequently achromogenic, sometimes it is isochromogenic. If the tumor grows endophytically it is most frequently isochromogenic in all parts. In our opinion the detection of low chromogenic (1 point according to Fleindler’s scale) areas in the tumor of urinary bladder is always indicative of infiltrating growth presence.
Tumor may be singular but tumors of urinary bladder most frequently have multifocal growth type up to total affection of the whole bladder. Detailed examination of all bladder walls is necessary because of this. Sizes, shape, chromogenecy and intensity of nodules invasion into the wall may be different in case of multifocal growth.
Major problems when performing NLS-research are faced when diagnosing the invasion into the submucous layer or when diagnosing the onset of invasion into the muscular layer. Spectral-entropy analysis often allows solving of such problems.
Tumors (especially endophytic ones) which affect major part of bladder wall may cause its sharp size reduction (microcystis). Small bladder capacity in such patients and also in patients who were surgically treated (often repeated due to repeated relapses) may complicate the detection of tumor’s invasion depth.
Urinary bladder tumors (more often multifocal) in combination with intravesical clots may be complicated for interpretation. Intravesical clots accompanied by macrohaematuria sometimes fill the whole bladder cavity. In these cases it is always possible to differentiate the tissue of the tumor nodule from clots using spectral-entropy analysis.
Diagnostic difficulties appear when detecting the depth of tumor invasion if the nodule is located in urinary triangle (Lieutaud body) especially when it overlaps on the contour of prostate gland. Image unsharpness of wall layers may be caused by multiple surgical interferences in case of bladder tumor relapses and also intravesical immune- or chemotherapeutical treatment and layering of urinary salts.
The sensitivity of NLS-method in detection of tumor invasion depth in such patients may be decreased.
Tumors coming from urachus must be described individually. When performing cystoscopic examination the tumors of urachus do not differ from a common bladder tumor. But certain difficulties may arise during NLS-research if one does not know the semiotics typical for urachus tumors. Urachus tumor is characterized by the location on the frontal wall in upper part of the bladder and also there is a presence of hyperchromogenic fibrotic fold (5-6 points according to Fleindler’s scale) of particular thickness that goes upwards, gradually narrows and binds the tumor with omphalus. It may seem as if tumor invasion spreads to adjacent tissues (however such tissues may not exist). Doppler sonography often detects intense blood flow both in tumor bottom and along fibrotic fold. During diagnostics of such tumor it is necessary to perform thorough examination to exclude premature metastasis in abdominal membrane, lymph glands and lungs.
Not only epithelial but also non-epithelial tumors may be found in urinary bladder. Despite the infrequency of such diseases the diagnosis may be presupposed during NLS-research based on typical ultramicroscopic picture. Preservation of complete or partial integrity of wall’s mucous layer is the particular feature of non-epithelial tumors. In this case the major part of the node is located in wall’s depth and beyond its borders.
Early relapse detection during case monitoring is one of the goals of NLS-research of patients who suffer from bladder tumors. Semiotics of relapsing bladder tumors in patients after organ preservation treatment does not have any fundamental differences from semiotics of primary tumors. Relapse of the tumor after cystectomy looks like nodus of increased chromogenecy of regular or irregular shape with even or uneven contour in bladder bed.
Metastatic affection of urinary bladder is possible (though quite rarely) besides presence of its primary tumors. There are 2 typical variants of NLS-graphic picture for metastases that go into bladder wall. The first one is round-shape tumor located in the wall’s depth with sharp smooth contour. Such variant resembles non-epithelial tumor judging by NLS-picture. The second variant (rarer type of metastasis) is the tumor that spreads on the wall; it resembles common picture of invasive cancer of urinary bladder. Information on anamnesis and also the results of spectral-entropy analysis allow correct diagnosing.
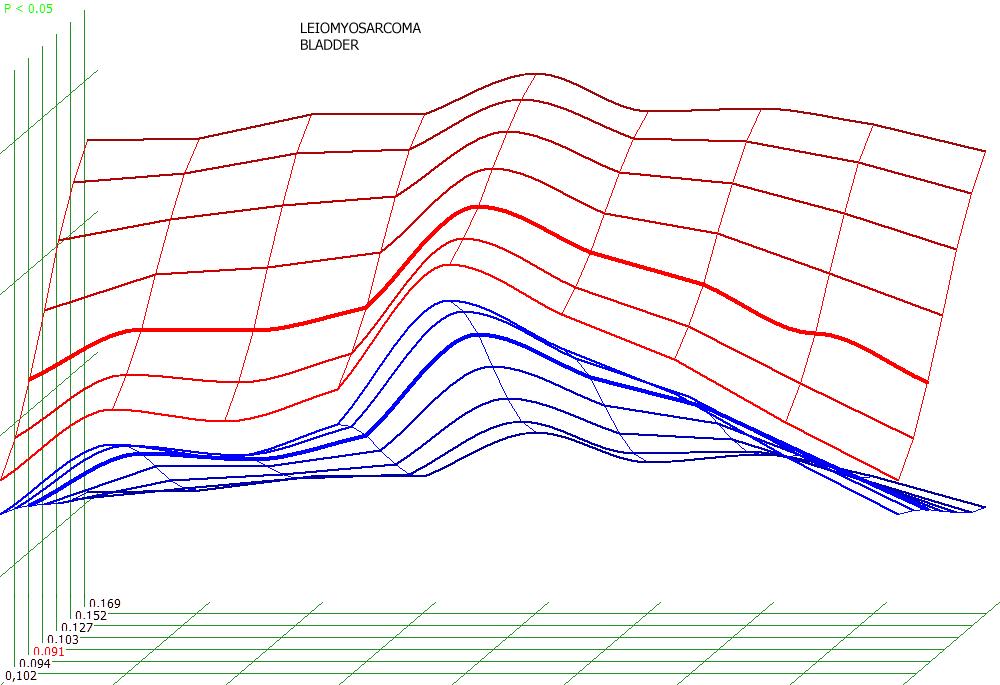
Рic. 3. Spectral-entropy analysis. Leiomyosarcoma of urinary bladder (D=0.091)
More occasional variant of secondary affection of the bladder that sometimes cause diagnostic difficulties is the intergrowth of tumors into wall of the bladder from the adjacent organs (most frequently it is cancer of large bowel, neck of womb or prostate gland). When tumor ingrows into the wall of the bladder this wall interrupts on the area that adjoins to the tumor and it is replaced by the tumor. Mucous layer may be preserved or the tumor that ingrows in it may press into the lumen of the bladder. If the tumor comes from large bowel then extraorgan tumor component that ingrows into urinary bladder changes to a typical symptom of the affected hollow organ. If the formation comes from the neck of womb then the tumor which is located in urinary bladder directly goes into changed neck. Nonorganic extraperitoneal tumors may seldom ingrow into the wall of urinary bladder.

Pic. 4. NLS-scanning. Cancer of the upper-and middle ampullar parts of straight intestine; ingrowth into urinary bladder.
Pic. 5. 3D NLS-graphy. Cervical cancer; ingrowth into urinary bladder.
The ingrowth into prostate gland is typical for tumors of urinary bladder located in the area of urinary triangle; and ingrowth into urinary bladder wall is typical for prostate gland tumors. Differential diagnostics of organ affiliation of prostate gland and urinary bladder tumors in case of ultramicroscanning has no real difficulties in 95% of patients. Although there may appear some diagnostic difficulties if the process is locally advanced and when urinary bladder in the area of urinary triangle and prostate gland (in rare cases when multifocal tumoral affection of both organs is present) are involved into this process.
In majority of cases the clinical picture in such patients does not allow performing differential diagnostics. Regardless of primary tumor localization there is distinct ankylurethria, often chronic urine retention (especially if the tumor developed in patient with benign prostatic hyperplasia), pain syndrome and macrohaematuria. Clinical picture does not exclude the possibility of prostate cancer and normal level of prostate-specific antigen. The increase of prostate-specific antigen is not an absolute diagnostic indicator of prostate cancer; although prostate-specific antigen is an organo-specific glycoproteid it is not OncoMarker itself.
We have performed a full-scale study (including 3D NLS-ultramicroscanning with spectral-entropy analysis and cystoscopy with targeted biopsy) of 28 patients with advanced cancer of urinary bladder who were treated by cystprostatevesiculectomy and 17 patients with advanced cancer of prostate gland detected by biopsy.
The analysis of NLS-picture in these patients was supplemented by spectral-entropy criteria of morphologic affiliation of the primary tumor. The following signs are the most significant ones in specification of primary process localization of large-scale urinary bladder tumors that ingrow into prostate gland:
1) localization of the maximum tumor component in urinary bladder;
2) multicentric affections of urinary bladder;
3) presence of the sharp edges between tumor and prostate gland contours.
The absence of abovementioned signs and localization of general tumor mass in gland itself are the most typical factors of prostate gland tumor.
Taking abovementioned signs into account allows accurate detection of which organ the locally advanced tumor comes out from – whether it is urinary bladder or prostate gland. The accuracy of the diagnostics of primary tumor site with consideration of these signs is 89.3%.
After performing of histological examination the multifocal synchronous tumoral process is found in 9 (32.1%) out of 28 patients with locally advanced cancer who had underwent surgery. These patients also suffered from localized prostate cancer besides urinary bladder cancer. The secondary tumor was diagnosed with the use of spectral-entropy analysis only in 1 of these patients.
As can be seen from the above the incidence of prostate gland cancer in these patients was the same as in elder men of full set population. Doctor was not searching secondary tumor in prostate gland because he was concentrated on solution of urinary bladder cancer prevalence problem. Obtained data demonstrates that prostate cancer must be excluded as much carefully than in elderly patients in general in case of advanced urinary bladder cancer.
2. The possibilities of various methods of NLS-research in case of urinary bladder tumors
The most statistically reliable method of NLS-research in case of urinary bladder tumors is an ultramicroscopic research with the usу of spectral-entropy analysis. Such method provides the detection of the tumor less than 3 mm., specifies its localization and in case of its invasive form it allows specifying its proportion in relation to adjacent organs and tissues. It is possible to examine the layers of bladder wall in all patients when using 3D NLS-ultramicroscopic research. We use spectral-entropy analysis in case of any process localization in urinary bladder after performance of ultramicroscopic research. Only endocavitary ultramicroscopic research is the most effective method for examination of all tumor aniages in case of multicentric growth.
The visualization of small sized formations (less than 4 mm.) is complicated in case of common non-scaling NLS-research; in more rarely cases the visualization of larger tumors located on the frontal urinary bladder wall is complicated. Performance of spectral-entropy analysis with ultramicroscanning always helps to make correct diagnosis in cases like these. The frontal urinary bladder wall which is put close to an abdominal wall is visualized with considerable zooming in, which allows examining both wall layers and their correlation with tumor nodule.
Common 2D NLS-research (which was put high hopes on) did not obtain widespread use in our country. Such method allows good visualization of superficial formations though relatively large ones (from 6-8 mm).
In case of deep invasion it is not always possible to estimate the exterior contour of the tumor. These peculiarities lower the effectiveness of 2D NLS-graphy method in detection of invasion depth into the bladder wall.
At the present time we are able to use extensively NLS-research of urinary bladder tumors with 3D reconstruction. The method allows visually presentation of the tumor and its correlation with surrounding tissues when making decision on choosing of surgical procedures type, and it allows storing the information in digital format.
Information storing provides the possibility for attending doctors to subsequently review the whole 3D information block which gives more objectiveness to 3D NLS-research.
CONCLUSIONS
1. Urinary bladder wall in 3D ultramicroscopic imaging has three-layer structure.
2. In case of urinary bladder cancer the common 2D NLS-research allows visualization of the tumor if its size is more than 5 mm. When performing 3D-ultramicroscopic research the tumors less than 2 mm. can be detected, it is also possible to define tumor’s growth form (exophytic, endophytic or combined one) and its invasion depth into the wall (prevalence of invasion influence both on disease prognosis and therapy method).
3. Major problems appear when diagnosing of initial tumor invasion into muscular layer. Ultramicroscanning with spectral-entropy analysis helps defining the depth of invasion when this occurs.
4. Familiarity with typical semiotics allows making the correct diagnosis when performing NLS-research in cases of non-epithelial tumors of urinary bladder and urachus tumors.
5. Information recording of anamnesis and performance of spectral-entropy analysis allow presupposing the correct diagnosis in case of metastases into urinary bladder wall of tumors of another primary localization.
6. Ultramicroscopic research with the use of spectral-entropy analysis allows specifying if the tumor which had been detected in urinary bladder emanates from the bladder wall or it is just a part of the tumor that emanates from other organs (large bowel, neck of womb, prostate gland and etc.) and ingrows into bladder wall.
7. To perform an appropriate diagnostics it is necessary to use all available NLS-research means considering the predisposition of urinary bladder tumor to multifocal growth.
8. Ultramicroscopic NLS-researches are the most effective ones when performing diagnostics of urinary bladder tumors. 3D reconstruction of the image increases both the effectiveness of diagnostics and it also provides more informative presentation of detected changes and it gives the possibility for reviewing of stored information.
9. In case of urinary bladder cancer it is necessary keep in mind the possibility of synchronous prostate cancer.
REFERENCES
1. Chissov V.I., Starinskiy V.V., Malignant growths in Russia in 2000 (disease and mortality rates), Moscow: MNIOI n.a. Gertsen P.A., 2002, p. 264.
2. TNM: Classification of malignant growth. 6th edition / Under the editorship of Blinov N.N., S-Petersburg.: Eskulap, 2003. p. 244.
3. Teplov A.A. Surgical and combination therapy of patients who suffer from invasive cancer of urinary bladder. Problem state. Choosing of treatment policy. // Materials of international scientific forum Oncology at the turn of XXI century. Prospects and possibilities. Moscow, 1999, p. 382-383.
4. Beer A., Saar B., Link T.M. et al. Virtual endoscopy of the urinary tract from T2-weighted and gadolinium-enhanced T1-weighted MR urographic images// Rofo. 2001.V. 173. №1. P. 997–1005.
5. Bernhardt T.M., Schmidl H., Philipp C. et al. Diagnostic potential of virtual cystoscopy of the bladder: MRI vs CT. Preliminary report // Eur. Radiol. 2003.V. 13. №2. P. 305–312.
6. Scher H.I., Shipley W.U., Herr H.W. Cancer of the Bladder // Cancer, Principles and Practice of Oncology. 5th ed. / Ed by De Vita V.T., Hellman S., Rosenberg S.A. Philadelphia: Lippincott Raven Publishers. 1997. P. 1300–1322.
7. Song J.H., Francis I.R., Platt J.F. et al. Bladder tumor detection at virtual cystoscopy // Radiology. 2001. V. 218. No.1. P. 95–100.
8. Yaman O., Baltaci S., Arikan N. et al. Staging with computed tomography, transrectal ultrasonography and transurethral resection of bladder tumour: comparison with final pathological stage in invasive bladder carcinoma // Br. J. Urol. 1996.V. 78. No.2. P. 197–200.
9. Mitina L.A. Ultrasonic diagnostics of urinary bladder new growths on different treatment stages: Thesis … MD, Moscow, 1998, p.108.
10. Mitina L.A., Kazakevich V.I., Stepanov S.O. Ultrasonic oncourology / Under the editorship of Chissov V.I., Rusakov I.G, Moscow: Mediya Sfera, 2005. p. 200
11. Sitdikov E.N., Sitdikova M.E., Zubkov A.Yu. Algorithm of ultrasonic monitoring of patients with urinary bladder new growths before and after surgical treatment. Kazan: Medicina, 1996, p 168.
12. Garin A.M. The secrets of prostate cancer, disputes on treatment of these patients // Material of VII Russian oncological congress. Moscow, 2003, p.28-32.
13. V.I. Nesterov. Computer nonlinear diagnostics. Collection of scientific papers of the Institute of Practical Psychophysics “Current problems of NLS-diagnostics”. Tome 1. Moscow. Katalog, 2006, p. 5-6.
14. V. Artukh, U. Shovkoplyas, A. Gavrilov. Computer non-linear analysis and its role in diagnostics. Collection of scientific papers of the Institute of Practical Psychophysics “Current problems of NLS-diagnostics”. Tome 1. Moscow. Katalog, 2006, p. 9-12.
15. V.I. Nesterov. 3D NLS diagnostics. Prospect of development. Collection of scientific papers of the Institute of Practical Psychophysics “NLS-diagnostics in medicine. Prospect of development”. Tome 3. Moscow. Katalog, 2010, p. 5-8.
16. Nesterova V.I., Shaposhnikov L.V., Yankina L.A., Kozhemyakin O.R. Application of NLS-diagnostics in oncology. New trends and prospects. // Collection of scientific papers of the Institute of Practical Psychophysics “NLS-diagnostics in medicine. Prospect of development”. Tome 3. Moscow. Katalog, 2010, p. 9-12
