Jackson S., Chang A.
University College London Hospital
Basing on the results of non-linear diagnostic examination of thorax of 267 patients suffering from purulent-destructive diseases of lungs and pleura we studied NLS-semiotics of lung abscess (112 patients), abscessed pneumonia (79 patients), pleural empyema (54 patients) and pulmonary gangrene (22 patients). We offered NLS-classification of lung abscesses based on a condition of their spontaneous drainage by bronchi, developed differential-diagnostic criteria of acute purulent and gangrenous abscesses. We singled out three NLS-variants of pulmonary gangrene: with large liquid-containing cavity, with numerous lesser cavities, with pyopneumothorax.
INTRODUCTION
Traditional roentgenologic methods still remain the basic in diagnostics of pulmonary organs diseases, but non-linear diagnostic research (NLS) of thorax organs opens conceptually new prospects for evaluation of lungs and pleura changes. Information about a pathological process is presented in a form of three-dimensional image with strict differentiation of various in spectral properties biological structures, at the same time application of ultramicroscopic scanning makes possible to study researched object in every detail. The study is not related to radiation exposure, it does not require expenses for additional equipment if a standard set of NLS-diagnostic devices is available. That is why at the present moment it finds more extensive application in diagnostics of lungs and pleura diseases and with increasing frequency becomes a topic of scientific works.
Until today NLS-semiotics and classification of lungs abscesses have not been developed, there are no strict criteria of their differential diagnostics.
The objective of this study is research NLS-semiotics of purulent-destructive diseases of lungs and pleura.
MATERIAL AND METHODS OF THE STUDY
We have examined 267 patients suffering from purulent-destructive diseases of lungs and pleura, who were treated in University College London Hospital, in 2009 – 2011. In accordance with a nosology all patients were divided into 4 groups named by the main disease: lung abscess (112 patients – 94 among them with acute abscess, 18 – with chronic one), abscessed pneumonia (79 patients), pleural empyema (54 patients) and pulmonary gangrene (22 patients). NLS-graphy data was verified by the results of surgical interventions, thoracic punctures with microbiological analysis of a punctate.
Thorax research was carried out using “Metatron”-4025 system (the IPP, Russia) with 4.9GHz high-frequency sensors in accordance with procedure created in the hospital.At visualization of pathological neoplasms we defined their localization, size, chromogeneity, spectral structure; applying spectral-entropic analysis (SEA) we evaluated changes of NLS-picture in dynamics. When there were pleural fluids we evaluated amount and structure of a fluid content with study of all inclusions (suspensions, threads) and condition of pleura. According to results of ultramicroscanning we judged about diagnostic value of each of mentioned criteria.
At the initial stage NLS-study of thorax was carried out after roentgenography with following comparison of results. Further on both diagnostic methods were applied simultaneously, but frequently NLS-study preceded roentgenography or replaced some part of it.
RESULTS OF THE STUDY AND DISCUSSION
NLS-semiotics of lung abscess
Pathomorphological basis and common NLS-symptom in patients with lung abscess was the presence of intrapulmonary cavity, the main diagnostic criteria of which were related to changing of chromogeneity of internal content and a wall. Spectral-entropic analysis helped to evaluate the content and its distribution in the cavity and thus to evaluate the efficiency of abscess spontaneous drainage through bronchi and decide if it was a purulent or a gangrenous form. Virtual visualization of walls was possible at chronic course of an abscess, thickness of walls and character of a contour were taken into consideration at differential diagnostics with cavernous form of peripheral lung cancer.
We singled out 4 types of acute lung abscess depending on efficiency of its spontaneous drainage through bronchi: blocked abscess, an abscess with insufficient spontaneous drainage, an abscess with free spontaneous drainage and an abscess with air pocket. These variants represent consecutive development steps of a nidal purulent-destructive process in a lung. Offered classification is based on differences in a structure of abscesses, namely on qualitative ratio of hypechromogenic purulent exudate (6 points at Fleindler’s scale) and achromogeneity of air inclusions (1 point) and a character of their spatial distribution in the cavity.
Blocked abscess was visualized as roundish neoplasm with hypechromogenic liquid content in which we detected isochromogenic suspensions (4-5 points at Fleindler’s scale), loosely distributed throughout a cavity of destruction (suppurative detritus), without achromogenic signals of air. At acute course a capsule of an abscess was not visualized. Purulent cavity was limited by lung parenchyma itself, which along with preserved air content was of the form of hypochromogenic line (2-3 points at Fleindler’s scale), but when air content was lost because of pneumonic infiltration, it was visualized as moderately chromogenic tissue (3-4 points). A width of this line varied depending on clarity of abscess limiting and significance of perifocal changes in a lung.
Burst of purulent content into bronchi meant start of open stage of abscess development with heterogeneous structure due to appearance of achromogenic signals against the background of hyperchromogenic fluid with suspensions. The efficiency of spontaneous drainage was evaluated by a quantity and a character of achromogenic inclusions (air) distribution in a purulent exudate. The drainage was considered insufficient at single or multiple lesser achromogenic cavities, diffusely distributed throughout the whole cavity of an abscess against the background of significantly prevailing hyperchromogenic content.
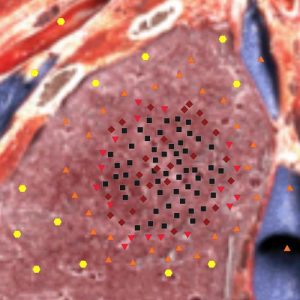
Pic.1. NLS-graphy. Blocked abscess of a lung. Heterogeneous hyperchromogenic suspensions in a cavity of an abscess.

Pic.2. NLS-graphy. Lung abscess with insufficient spontaneous drainage. Multiple achromogenic nidi because of air beads.
An abscess with air cavity was registered after cleaning out of purulent exudate from remained cavity of destruction with formed solid capsule. In the spot where it touches a thoracic wall we detected arcual strip with uneven, jugged surface. To evaluate such air cavities roentgen examination is preferable, because it allows to visualize the whole cavity, not only a mural spot.
In case of cleaned cavity collapse and at its cicatrization, at the place of an abscess was formed a fibrous area of irregular shape with uneven and indistinct contours and isochromogenic structure because of separate hyperchromogenic inclusions against the background of moderately chromogenic fibrous tissue. Maximum size of such area was less than 2 cm. At significant adhesive changes at the level of an abscess locally thickened hyperchromogenic pleura (4-5 points at Fleindler’s scale) of up to 6 mm was visualized.
We have carried out comparative analysis of 62 acute purulent and 32 gangrenous abscesses and defined criteria for their differential diagnostics, which were: efficiency of spontaneous drainage, presence of hyperchromogenic wall and necrotized sequesters of lung tissue. All patients suffering from gangrenous abscesses were subjected to surgical treatment (thoracoabscessotomy), that allowed to evaluate visually macroscopic structure of purulent cavity. Comparison with acquired NLS-picture we singled out early and advanced stages of gangrenous abscess, associated with various efficiency of spontaneous drainage and presence of a wall.

Pic.3. NLS-graphy. Lung abscess with free spontaneous drainage. Achromogenic nidi due to presence of air in an upper part of an abscess; hyperchromogenic liquid content with heterogeneous suspensions in lower parts of a cavity.
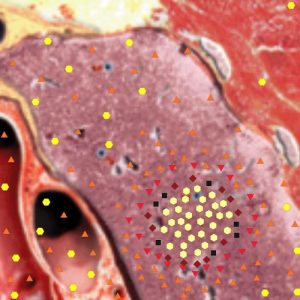
Pic.4. NLS-graphy. Lung abscess with air cavity. Achromogenic air cavity of an abscess; hyperchromogenic wall.
Macroscopic basis of an early stage was a large cavity of destruction with insufficient spontaneous drainage, indistinctly separated from surrounding lung tissue and filled with purulent exudate with sequesters (25 patients). On NLS-graphy early stage was characterized by a neoplasm with heterogeneous structure due to diffuse distribution of lesser achromogenic areas of air beads against the background of prevailing isochromogenic content with heterogeneous suspensions and presence of large hypochromogenic sequesters. Walls were not visualized, abscess was separated by lung tissue.
At the advanced stage we detected cavity of destruction with solid walls, properly drained by bronchi and containing mainly air, sequesters and small amount of purulent exudate (7 patients). On NLS-graphy it was characterized by heterogeneous neoplasm with prevailing long achromogenic objects with small amount of fluid in lower parts. Also homogeneous moderately chromogenic abscess wall of equal thickness with distinct external and indistinct internal walls was visualized.
Acute purulent processes are characterized by smaller than gangrenous abscesses size, often insufficient spontaneous drainage with heterogeneous diffuse distribution of achromogenic inclusions of air against isochromogenic background, absence of walls and sequesters. At adequate treatment we detected a positive dynamics in form of abscess cavity decreasing with simultaneous decreasing of fluid content amount and replacing by air. Further on a cicatrix was formed at the spot.
Chronic lung abscesses are characterized by the same regularities of NLS-picture as acute ones. Diagnostic criteria are the quantitative ratio of purulent exudate and achromogenic air inclusions and their spatial distribution in a cavity. We singled out 4 types of chronic abscess depending on efficiency of its spontaneous drainage through bronchi: without access to bronchi (pseudo-tumorous), with insufficient spontaneous drainage, with free spontaneous drainage and an abscess with air pocket.
The main difference between chronic abscess and acute one was a presence of moderately chromogenic wall which was more distinctly visualized at the level of air content in the upper part of a cavity and less distinctly – in the lower part against the background of hyperchromogenic purulent exudate with suspensions. A wall had homogeneous chromogenic structure (4 points at Fleindler’s scale), even thickness (up to 8 mm), distinct external and indistinct internal contours.
The greatest diagnostic difficulty was represented by pseudo-tumorous form of chronic abscess, which had, as a rule, homogeneous hyperchromogenic structure because of dense purulent content and distinct contour imitating peripheral lung cancer. Etiology of a nidus was defined by SEA results and confirmed by puncture biopsy.
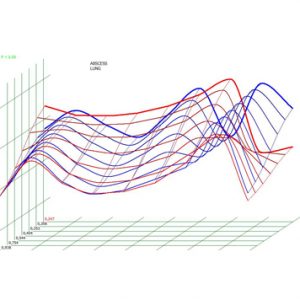
Pic.5. Spectral-entropic analysis. Lung abscess (D=0,247).
NLS- semiotics of abscessed pneumonia
In the group of patients suffering from abscessed pneumonia a pathomorphological basis of a picture was presence of interalveolar exudation and inflammatory infiltration. Fibrinous exudate in alveoli allowed to scan pneumonic infiltrate down to the depth, which was the distinctive feature of the whole group.
Quantity and character of hyperchromogenic inclusions distribution mainly depended on severity of pneumonic infiltration, nominally divided into massive, significant and moderate.
Pulmonic fever with massive inflammatory infiltration had almost homogeneous moderately chromogenic structure (4-5 points at Fleindler’s scale) with single lesser hyperchromogenic areas in a root zone. At significant infiltration a number of hyperchromogenic areas was greater, but they were located heterogeneously and between them there were homogeneous hyperchromogenic areas. Moderate inflammatory infiltration was characterized by multiple diffusely located hyperchromogenic inclusions.
Absence of hyperchromogenic line in pneumonic infiltrates allowed to visualize on their surface a visceral pleura, on the internal surface of thoracic wall – a parietal pleura. Pleural fluid led to appearance of a hyperchromogenic space with separation of pleural slips between a lung surface and thoracic wall. Fibrinous pleural imbrications were of form of isochromogenic imbrications with uneven jugged surface.
Presented picture of pulmonic fever was a background against which destructive changes of pulmonary tissue developed. Their NLS-semiotics depended on size and efficiency of spontaneous drainage of decay cavities, that is why the same stages as of lung abscesses were singled out.
Closed decay cavities at abscess forming pneumonia were visualized rarely, because at destruction of a lung tissue burst of purulent exudate into bronchi happened early.
As a rule, destruction nidi were of form of several lesser (size up to 2 cm) closely located hyperchromogenic areas of irregular shape with uneven and indistinct contours. Further on at this spot a single cavity with air and fluid contents was formed. It had no own walls and was limited by infiltrated parenchyma of lung itself.
At insufficient spontaneous drainage, in a cavity prevailed hyperchromogenic exudate with separate achromogenic air inclusions, diffusely or parietally located along a border with a lung tissue. Due to mural gaseous inclusions, a contour of the destruction area was outlined by short achromogenic lines.
At free spontaneous drainage in decay cavities there was air mainly, that is why they were visualized as achromogenic areas in the structure of hyperchromogenic pneumonic infiltrate. Strictly limited major air cavities had a form of achromogenic arc, lesser ones – homogeneous achromogenic areas of oval shape.
Presence of a small amount of detritus and purulent secretion mixed with air in the destruction cavity provided isochromogenic mosaic-like structure and indistinct contours to its content.
NLS-semiotics of pleural empyema
In the group of patients suffering from pleural empyema there were 54 patients with purulent exudate in a pleural cavity. In 43 patients we registered limited exudate of oval shape with paracostal localization, often along posterior or lateral surface of thorax. In 11 patients pleural empyema was of diffused character, in 6 of them pyopneumothorax was diagnosed. In 39 patients had para- and metapneumonic genesis, in 8 patients – posttraumatic, it 7 reason was not found.
The main diagnostic criterion of pleural empyema was hyperchromogenic suspension caused by purulent detritus. In the majority of cases it was spread throughout the whole volume of empyemic cavity, had high density, heterogeneous character and it could imitate a solid neoplasm. To differentiate it with a tumor a spectral-entropic analysis must be applied. There were no isochromogenic fibrinous fibers in an empyemic cavity, it was limited by thickened pleura slips (up to 8 mm) with uneven surface.
In single cases purulent content in pleural cavity had lamellar character with hyperchromogenic areas of various shapes. Heterogeneous structure of pleural empyema with more chromogenic, than suspension itself, fragments with uneven contours was registered at hemopleura suppuration, when partially decayed thrombotic clots were found in purulent content.
At pyopneumothorax we detected major diffusely located achromogenic areas corresponding to a separate air beads in purulent exudate. Depending on size they had a form of both point inclusions and quite extensive neoplasms. Free air in pleural cavity caused appearance of achromogenic line above fluid content.
NLS-semiotics of pulmonary gangrene
NLS-semiotics of pulmonary gangrene differed by significant diversification of a picture due to spreading of purulent-destructive process to the whole lung with involvement of pleura and, as a result, a combination of various NLS-symptoms.
Analysis of NLS-image was carried out taking into account the whole clinical picture. After taking as a basis of classification the leading symptom we nominally singled out three NLS-variants of gangrene. At the first variant (11 patients) in a lung against the background of massive inflammatory infiltration we detected a major cavity of destruction with mainly liquid content, NLS-picture was analogous to gangrenous abscess with insufficient spontaneous drainage. Walls of a cavity were not visualized, it was limited by lung parenchyma, in certain areas the line between them was indistinct.
At the second variant (7 patients) in the picture prevailed total thickening (accompanied by increasing of chromogeneity) of a lobe or the whole lung with presence of multiple roundish achromogenic areas due to lesser air cavities of destruction. In 3 patients, apart from air cavities, there were hyperchromogenic fluid-containing cavities of decay (6 point), in one patient they prevailed in the structure of gangrenous lung. In 8 of 18 patients with first two variants of gangrene a pleural empyema with the typical picture appeared.
The third variant of lung gangrene (4 patients) had a course with development of pyopneumothorax, when a massive pleural fluid with heterogeneous suspension and achromogenic inclusions of air was the leading echo-symptom. Gangrenous changes in a pulmonary tissue were characterized by one of above mentioned variants: a major cavity with purulent content of multiple lesser nidi of destruction.
Thus, NLS-research of thorax is an informative, radiologically safe method of purulent-destructive lungs and pleura diseases diagnostics, allowing to not only acquire additional information, but to carry out primary examination and dynamic monitoring. NLS-semiotics of pathological changes in a lung is diverse and depends, first of all, on focal or diffuse character of lung affection. Analysis of NLS-picture makes possible to define a character and severity a purulent-destructive process in a lung (acute purulent or gangrenous abscess, abscess forming pneumonia, gangrene), its spreading to pleural cavity (empyema, pyopneumothorax). The common factor, which determines NLS-picture of purulent cavity at abscess and abscess forming pneumonia, is a condition of its spontaneous drainage, which is evaluated by quantity and character of distribution of achromogenic air areas in a cavity. The main symptom of pleural empyema is a presence of a thick chromogeneous suspension in pleural fluid; at pyopneumothorax achromogenic air areas appear. NLS-semiotics of gangrene is quite diverse due to the greatest severity of destructive changes and is formed by focal and diffuse changes in a lung, although its clinical course may be characterized by prevalence of one of these variants.
REFERENCES
1.Eibenberger K.L., Dock W.I., Ammann M.E. et al. Quantification of pleural effusions: sonography versus radiography // Radiology. 1994.V. 191. №3. P. 681–684.
2.Gehmacher O., Kopf A., Scheier M. et al. Can pleurisy be detected with ultrasound? // Ultraschall Med. 1997.V. 18. №5. P. 214–219.
3.Targhetta R., Bourgeois J.M., Marty-Double C. et al. Peripheral pulmonary lesions: ultrasonic features and ultrasonically guided fine needle aspiration biopsy // J.Ultrasound. Med. 1993.V. 12. №7. P. 369–374.
4.Yang P.C., Chang D.B., Yu C.J. et al. Ultrasound-guided core biopsy of thoracic tumors // Am. Rev. Respir. Dis. 1992.V. 146. №3. P. 763–767.
5.Yang P.C., Luh K.T., Lee Y.C. et al. Lung abscesses: US examination and US-guided transthoracic aspiration // Radiology. 1991.V. 180. №1. P.171–175.
6.Mathis G., Gehmacher O., Kopf A. et al. Lungenabszess–Ultraschallgefьhrte Drainage // Ultraschall Med. 1995. Bd. 16. №1. S. 60.
7.Sakai F., Sone S., Kiyono K. et al. High resolution ultrasound of the chest wall // RoFo. 1990.V. 153. №4. P. 390–394.
8.Mathis G.Lungen- und Pleurasonographie. Berlin, Heidelberg, New York: Springer-Verlag, 1996. 117s.
9.Kroegel C., Reiig A.Transthorakale Sonographie: Grundlagen und Anwendung; ein Leitfaden fr die Praxis. Stuttgart, New York: Thieme, 2000. 116 s.
10.Görg G.Lunge // Sonographische Differenzial-diagnose / Hrsg. von Schmidt G.Stuttgart, New York: Thieme, 2002. S.487–507.
11.Anzbock W., Stellamor K., Braun U., HrubyW.Sonography of the lungs and pleura // RoFo. 1990.V. 153. №3. P. 278–282.
12.Mathis G., Metzler J., Fussenegger D. et al. Ultraschallbefunde bei Pneumonie // Ultraschall Klin. Prax. 1992. Bd. 7. №1. S. 45–49.
13.Yang P.C., Luh K.T., Chang D.B. et al. Ultrasonographic evaluation of pulmonary consolidation // Am. Rev. Respir. Dis. 1992.V. 146. №3. P. 757–762.
14. S.N. Makarova. NLS-diagnostics of lung abscess // Collection of scientific works of the Institute of Practical Psychophsics “Actual issues of NLS-diagnostics”. Tome 1. Moscow: Katalog, 2006, p. 27-29.
15. V.I. Nesterova, T.G. Kuznetsova, N.L. Ogluzdina. NLS-diagnostics of diffuse infiltrative lung diseases // Collection of scientific works of the Institute of Practical Psychophsics “Actual issues of NLS-diagnostics”. Tome 1. Moscow: Katalog, 2006, p. 34-39.
